Introduction
Pulmonary emboli are blood clots. They usually form in leg veins or in pelvic veins, break loose and end up in the lung vessels.
Clots happen because a person is particularly vulnerable from a constitutional point of view. However, a patient following surgery has thicker blood for a period of time and clots happen easier. A woman on the birth control or as a result of hormone replacement with Provera can also get clots.
Clots in leg veins can become pulmonary blood clots
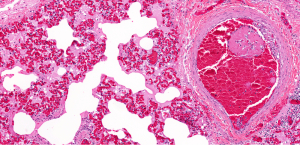
When clots occur in leg veins or pelvic veins, there is a risk that the clots grow. Eventually they break off and migrate into the right heart. There they tend to break up and move on into the arteries of one or both lungs (see how this affects the lung).
This can lead to acute symptoms and in about 10% of the cases is severe. It can close off the circulation to at least a part of the lung (if not all of the lung). Physicians call this pulmonary infarction. When clots from the veins in the legs break off and migrate into the lungs pulmonary emboli result. In about 65% this affects both lungs. There are anatomical differences, which lead to slightly more blood circulation to the right lung. This is why 25% of cases occur in the right lung and 10% in the left lung.
Signs and symptoms
The onset of pulmonary emboli is usually very acute. There are a variety of symptoms that occur simultaneously. The most striking symptom is an air hunger and rapid deep breathing (dyspnea).
If the clots are massive, the patient may get into shock and become unconscious or may even die. However, this happens only in 1 to 5%. Here are some of the most common symptoms of blood clots. Most of the time there is a slower onset or there is only a partial blockage of the pulmonary arteries. But the patient still requires transportation to hospital by ambulance as quickly as possible. The physician starts heparin, an anticoagulant medication right away to prevent further clot formation. The healthcare provider starts other clot dissolving medication as well to get a rapid improvement of the condition as soon as possible.
Friction rubs, hemoptysis and other symptoms
With clots that lead to infarction at the surface of the lung there will be a friction rub that the doctor may hear using the stethoscope and the patient feels pain with every breath due to pleuritic pain. Hemoptysis (coughing up blood or blood-stained phlegm) can be another sign as well as wheezing. The patient is usually extremely anxious and restless, which may be in part due to a lack of oxygen in the brain. There is a list of other symptoms in the table below.
Symptoms of Pulmonary Emboli (PE)
| Symptom: | Frequency: |
| dyspnea | 73%* |
| pleuritic pain | 46% |
| cough | 43% |
| leg swelling | 33% |
| leg pain | 30% |
| hemoptysis | 15% |
| palpitations | 12% |
| wheezing | 10% |
| angina type pain | 5% |
*Note: %-ages do not add up to 100%; symptoms can occur simultaneously
Diagnostic tests
A patient with pulmonary emboli needs to be seen and treated in the Emergency Department of a hospital. Several tests need to be done in rapid succession and heparin and clot dissolving therapy needs to be started at the same time.
After a quick examination the Emergency Room physician likely will want to do some simple initial tests such as oximetry on a finger or ear lobe and spirometry.
Initial tests involve arterial blood gases
Arterial blood gases likely will also be obtained right away as this is giving the physician a good initial assessment as to how extensive the clots in the lungs are. A very low partial oxygen pressure in the blood likely is associated with a lot of clots affecting the oxygen absorption significantly. A chest X-ray and likely will be ordered. The lung perfusion scan is done with radioactive tracer substances (with the radioisotope technetium 99m) and is probably the most important of the tests. It measures the lack of perfusion in the lung tissue affected by pulmonary emboli. The series of scans depicted under this link show a sequence of normal scans in the upper area. In the lower half of the link abnormal perfusion scans demonstrate a large pulmonary embolus in the right lung of this patient.
Ventilation perfusion scan
Another type of lung scan, the ventilation perfusion scan uses the inhaled gas xenon-133, which measures the air flow into the lungs. When the lung perfusion and the lung ventilation scans are done simultaneously, the result shows by way of subtraction where a perfusion defect is located. The corresponding lung tissue, which is now blocked by clots from receiving blood from the affected lung artery branch, is still ventilated normally in this area, except for the area where a lung infarction has developed. That’s why about 90% of the cases with pulmonary emboli can be diagnosed this way with confidence, which is considered to be a very reliable test.
Pulmonary arteriogram (or angiogram) and other tests
For the remaining difficult cases where clinically the patient appears to have pulmonary emboli, but the imaging studies do not clearly show the clots in the lungs, the physician may want to consider a pulmonary arteriogram (or angiogram) to show an arterial filling defect where the clot is located. Further tests such as CT scans, CT pulmonary angiography and MRI scans can be done to get more details as well, if the extent of the clots needs to be determined.
Treatment
Treatment depends on the clinical presentation and the finding of the tests in a particular patient. However, generally speaking a form of clot dissolving treatment (thrombolytic therapy) is chosen.
There are rapidly dissolving therapies such as streptokinase and plasminogen activating (t-PA) substances. Then there is clot prevention therapy utilizing heparin initially and a few days later a switch to oral medication such as warfarin. Medical commissions developed exact protocols to standardize the anticoagulatory treatment and to avoid over-treatment. Over thinning the blood can cause major bleeding in various areas (brain hemorrhage, seriously bleeding ulcers etc.). With deep vein thrombosis following surgery often the patient will be treated with warfarin for extended periods such as 3 to 6 months to avoid a recurrence of clots. People with atrial fibrillation who have an ongoing risk for blood clots may have to stay on warfarin lifelong.
Low molecular weight heparins
The newest development in treating pulmonary emboli and other clots is by way of the use of low molecular weight heparins. Various commercial preparations are available (Dalteparin, Enoxaparin, Nadroparin and Tinzaparin are pharmacological names). They all have different brand names as well. The dosage is different for each product as the metabolic half-life is unique for each product.
Switch to Coumadin before discharge from hospital
However, it is now recognized by the medical profession that these low molecular heparins are very safe and very effective. The advantage is that they work very quickly in dissolving the clot. Once the patient has been started on it and the doctor knows whether the patient tolerates it and how it thins the blood, no further tests for monitoring have to be done. With regular heparin in the hospital setting or Coumadin in the home setting blood tests have to be done frequently to check the degree of blood thinning. The disadvantage is that the patient has to inject a little needle with the low molecular weight heparin into rotating spots of the skin on a regular basis (e.g. twice per day). Small amounts of aspirin can also be combined with low molecular weight heparin (Ref. 10).
References
1. Noble: Textbook of Primary Care Medicine, 3rd ed., Copyright © 2001 Mosby, Inc.
2. National Asthma Education and Prevention Program. Expert Panel Report II. National Heart, Lung and Blood Institute, 1997.
3. Rakel: Conn’s Current Therapy 2002, 54th ed., Copyright © 2002 W. B. Saunders Company
4. Murray & Nadel: Textbook of Respiratory Medicine, 3rd ed., Copyright © 2000 W. B. Saunders Company
5. Behrman: Nelson Textbook of Pediatrics, 16th ed., Copyright © 2000 W. B. Saunders Company
6. Merck Manual : Pulmonary embolism
7. Goldman: Cecil Textbook of Medicine, 21st ed., Copyright © 2000 W. B. Saunders Company
8. Ferri: Ferri’s Clinical Advisor: Instant Diagnosis and Treatment, 2004 ed., Copyright © 2004 Mosby, Inc.
9. Rakel: Conn’s Current Therapy 2004, 56th ed., Copyright © 2004 Elsevier
10. Dr. Linda Vickars (Head, Div. of Hematology, Providence Health Care, Vancouver/BC and UBC Associate Professor of Medicine) at The 50th Annual St. Paul’s Hospital Continuing Medical Education Conference for Primary Physicians, Nov. 16 – 19, 2004
11. Suzanne Somers: “Breakthrough” Eight Steps to Wellness– Life-altering Secrets from Today’s Cutting-edge Doctors”, Crown Publishers, 2008