Introduction
This group of lung diseases is very common in industry. But occasionally people or employers do not recognize it, particularly if the person is also a smoker.
There are many forms of dust at various workplaces, some are organic, some inorganic (metal). In the case of exposure to organic substances the resulting lung diseases has the name “pneumonitis”.
Some individuals are more sensitive than others. They develop a hyper-reactivity through the production of antibodies. This occurs due to sensitization of immune cells to the organic compounds. The name for this condition is “hypersensitivity pneumonitis”. In the case of exposure mainly due to non-organic substances the occupational lung disease has the name pneumoconiosis. I discuss this further below.
Occupational lung diseases
| Name of disease: | Description of exposure: |
| air conditioner lung | similar to farmer’s lung, from mold spores in the air conditioner ducts |
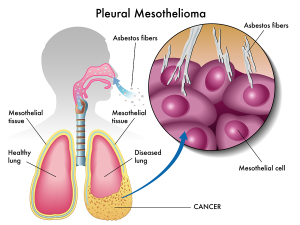
| asbestosis | from longterm exposure to asbestos dust being incorporated into lung tissue |
| berylliosis | only 2% of persons, exposed to beryllium dust, get it; today mostly in aerospace industry |
| byssinosis | exposure to cotton, hemp or flax dust causes bronchoconstriction |
| Caplan’s syndrome | coal dust exposure in patient with rheumatoid disease develops this acute nodular lung disease |
| coal workers’ pneumonitis (CWP), also called “black lung disease” | about 1 to 2% of coal mine workers exposed to coal dust develop progressive massive fibrosis(PMF) |
| exposure to irritant gases | accidental exposure to chlorine, sulfur dioxide, nitrogen dioxide, ammonia, hydrogen sulfide and other gases can lead to acute lung damage |
| humidifier fever | toxins from bacteria, fungi or amebas can cause a flu-like illness with breathing problems |
| red cedar dust asthma | red cedar dust can cause acute asthma and lung fibrosis in sensitized patients |
| sick building syndrome | airtight buildings can cause elevated CO2 levels, aggravated by truck exhausts idling near air vents adding noxious gases (nitrogen oxide, carbon monoxide, aldehydes and other irritants) |
| silicosis | silica dust exposure from pottery work, from mining for silver, gold, copper, hard coal and lead, but also from sandblasting or granite cutting etc. A late complication is malignant mesothelioma. |
Particle size of inhaled compound important
Generally speaking, the further a chemical compound can invade into the airways or lung tissue, the more serious the tissue reaction.
It depends also on the reactivity of the chemical that intrudes and on the concentration and length of exposure. With silicosis special clean-up cells with the name “macrophages”, try to engulf and inactivate the silica particles. However, they fail and die off. In this process there is a release of lytic enzymes that damage the surrounding lung tissue. This leads to a fibrotic tissue reaction that narrows the airway passages severely. The end result is a nodular lung fibrosis.
Lung biopsy and special examination under microscope
The pathologist stains a lung biopsy with special stains. Subsequently he views it under polarized light, which shows rust colored silica bodies. Asbestos exposure leads to a diffuse interstitial fibrosis (=asbestosis). The pathologist can detect this due to needle like asbestos fibers. He uses iron stain histology slides of a lung biopsy as shown here. Unfortunately very little can be done after the damage of many years of exposure to these substances.
Prevention of exposure to noxious substances is the key to avoiding the devastating effects of lung fibrosis
There are some substances, which are inert. For instance, exposure to iron oxide, tin or barium dust leads to siderosis, baritosis and stannosis. This lung X-ray picture of a patient with siderosis looks as if the patient should have breathing problems. However, the patient has absolutely no symptoms and no disability as iron oxide is a substance that is inert with no effect on lung tissue other than showing up on these diagnostic tests. The same is true for baritosis and stannosis. Here is an overview of a selection of common occupational lung diseases with links to sites that give you more details regarding symptoms, diagnosis and treatment.
Signs and symptoms
Symptoms vary from case to case and within a patient group tend to be more symptomatic after a lengthy exposure (15 to 20 years or more) to high concentrations of dust. At the same time symptoms are much more prominent, if the patient has also been a heavy smoker or has had exposures to other noxious substances that have led to chronic bronchitis or emphysema. The exposure to cigarette smoke also predisposes the patient to lung cancer, the symptoms of which would be overlapping.
Shortness of breath on exertion
Generally speaking, shortness of breath on exertion and a chronic cough as well as a cyanotic (bluish tinge) skin discoloration are the hallmarks of this patient group at the later stages. However, a non-smoker who has simple nodular silicosis, or simple coal workers’ pneumoconiosis (CWP) would not have any lung symptoms and only show up abnormally on tests such as pulmonary function tests or X-rays. Details about the above-mentioned diseases can be found under the various links.
Diagnostic tests
A patient who is getting symptoms of coughing up phlegm and getting short of breath when walking uphill on a slight incline where he was asymptomatic before, needs a few screening tests done. Chest X-rays are a starting point along with a thorough examination by a physician to check this patient out who who has had perhaps a 20 year dust exposure working in a coal mine. Such a patient may have this X-ray finding of the lungs. As the findings are rather extensive, further investigations with a CT scan and bronchoscopy have to be done by the lung specialist to rule out lung cancer.
A case of tuberculosis with exposure to silica dust
In a case where it was thought that the patient was cured from a previously treated tuberculosis, and who was symptom free for years, the patient came down with new symptoms. Chest X Ray, CT scan and bronchoscopy were all done. After the biopsy material came back from the pathologist it was noted that the patient had silico-tuberculosis. Exposure to silica dust makes the patient much more vulnerable to contract tuberculosis and it is a much more chronic form of this disease. Silicosis is also associated with malignant mesothelioma, an otherwise rare lung tumor of the pleural surfaces.
Treatment
Unfortunately there is no specific treatment for any of the occupational lung diseases. Treatment is directed at making the patient’s breathing more comfortable, but the overall outlook (prognosis) is not changed. The most important step in the therapy is to convince those who are still exposed to toxic substances for the lungs, to remove this exposure. This includes a stop smoking program and early retirement from the job that caused the disease. It may be that Workers’ Compensation is at least partially liable and depending on the jurisdiction this may involve some possible legal action. A last resort, for those short of breath, is using continuous oxygen.
References
1. Noble: Textbook of Primary Care Medicine, 3rd ed., Copyright © 2001 Mosby, Inc.
2. National Asthma Education and Prevention Program. Expert Panel Report II. National Heart, Lung and Blood Institute, 1997.
3. Rakel: Conn’s Current Therapy 2002, 54th ed., Copyright © 2002 W. B. Saunders Company
4. Murray & Nadel: Textbook of Respiratory Medicine, 3rd ed., Copyright © 2000 W. B. Saunders Company
5. Behrman: Nelson Textbook of Pediatrics, 16th ed., Copyright © 2000 W. B. Saunders Company
6. Merck Manual: Environmental Lung Diseases
7. Goldman: Cecil Textbook of Medicine, 21st ed., Copyright © 2000 W. B. Saunders Company
8. Ferri: Ferri’s Clinical Advisor: Instant Diagnosis and Treatment, 2004 ed., Copyright © 2004 Mosby, Inc.
9. Rakel: Conn’s Current Therapy 2004, 56th ed., Copyright © 2004 Elsevier