Introduction
A pneumothorax means literally “air in the chest”. The only problem is that the air this time is not in the lungs, but in the pleural space. The location of the pleural space is between the surface of the lung and the lining of the chest cavity. There is normally no air there, but just a bit of slippery fluid.
This way the pleural layer on the lung surface and the pleural layer inside the chest wall have an attachment to each other by strong adhesive forces. However, the adhesive forces still allow the lungs to move freely with every breath we take. A stab wound injury through the full thickness of the chest wall disturbs the integrity of the pleural mechanism.
How a pneumothorax develops
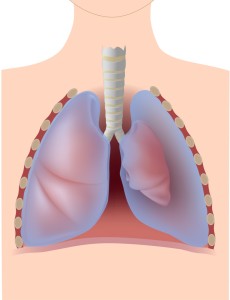
The recoil of the lung tissue from the elastic tissue in the lung collapses part or all of the lung and air gets sucked in creating the pneumothorax. The illustration on this page shows schematically what happens without the gory details you would see as a physician in the Emergency Room of a hospital.
Emphysematous patients can develop pneumothorax
In emphysematous patients there often is an emphysematous bleb (an air-filled thin blister that can easily break). Usually you find this in the upper lung regions. Tall men, often younger than 40 years of age, can get a “spontaneous” pneumothorax with no apparent cause. A more sinister cause can be a tumor in the bronchial tube (lung cancer) where the tumor creates a connection between the air from the bronchial tree and the pleural space resulting in a pneumothorax as well. Occasionally a procedure such as a central intravenous line can cause a pneumothorax as well, which is why physicians usually do a chest X-ray after completion of the procedure to check this out.
Signs and symptoms
The patient is suddenly short of breath and likely also complains of chest pain due to the irritation of the very sensitive pleural surfaces by air. The physician may miss a minor pneumothorax. But chest X-rays for cough from a cold, where the doctor wants to rule out pneumonia sometimes show pneumothorax. With a larger pneumothorax the patient may complain of a dry, hacking cough and heart palpitations may be present. In a large pneumothorax where most of the lung is collapsed, the circulatory symptoms may be in the foreground with a sudden collapse and serious breathing problems. There is a particularly serious pneumothorax, where a valve mechanism develops. With every breath the patient takes, more air gets pumped into the pneumothorax leading to a tension pneumothorax.
Diagnostic tests
The patient with a pneumothorax usually has less chest wall movements on the affected side. There may or may not be a lack of oxygen when an arterial blood gas is taken. Chest X-rays show a lack of lung markings on the side where the pneumothorax is. The physician has to specifically look for this in more subtle cases. Auscultation (stethoscope) often reveals to the physician a lack of breath sounds on the affected side.
Treatment
The treatment for a pneumothorax is usually a chest tube for a few days in the hospital setting until the hole in the lung seals itself as shown on this link. The chest tube is hooked up to a vacuum, which facilitates re-expansion of the lung. Within a short period of time (1 to 3 days) the cardiovascular status tends to stabilize and the patient is ready for discharge home within less than a week from the date of the hospital admission. In the case of lung cancer the patient has to see a cancer specialist. When an emphysematous bleb is present at the top of the lung, the cardiovascular surgeon resects this through thoracoscopy. This is essentially a “chop-stick” surgical setup, which removes the emphysematous bleb through holes. A laparoscopic procedure is much less invasive than the traditional open procedure.
Video-Assisted Thoracoscopic Surgery (VATS)
In the case of a minor to midsize lung surgery procedure this can be done with a stapling device through thoracoscopy chest wall openings. The patient recovers from this surgical laparoscopic procedure (also called video-assisted thoracoscopic surgery) much faster. In the past the chest surgeon did a conventional thoracotomy procedure where he cut open the chest cage.
References
1. Noble: Textbook of Primary Care Medicine, 3rd ed., Copyright © 2001 Mosby, Inc.
2. National Asthma Education and Prevention Program. Expert Panel Report II. National Heart, Lung and Blood Institute, 1997.
3. Rakel: Conn’s Current Therapy 2002, 54th ed., Copyright © 2002 W. B. Saunders Company
4. Murray & Nadel: Textbook of Respiratory Medicine, 3rd ed., Copyright © 2000 W. B. Saunders Company
5. Behrman: Nelson Textbook of Pediatrics, 16th ed., Copyright © 2000 W. B. Saunders Company
6. Merck Manual : pneumothorax
7. Goldman: Cecil Textbook of Medicine, 21st ed., Copyright © 2000 W. B. Saunders Company
8. Ferri: Ferri’s Clinical Advisor: Instant Diagnosis and Treatment, 2004 ed., Copyright © 2004 Mosby, Inc.
9. Rakel: Conn’s Current Therapy 2004, 56th ed., Copyright © 2004 Elsevier
10. Suzanne Somers: “Breakthrough” Eight Steps to Wellness– Life-altering Secrets from Today’s Cutting-edge Doctors”, Crown Publishers, 2008