In the first place, there are four different types of thyroid cancer, which I am reviewing here. In general, the biopsies and the resulting histopathology findings determine what category of thyroid cancer the patient has. To emphasize, there are 4 different thyroid cancer types. For this reason, it is important for the cancer specialist to distinguish between these subtypes of thyroid cancer as the growth patterns are different. To clarify, the responses to various therapeutic modalities are also quite different depending on what histological type the patient has. The pathologist reviews the histological material of the biopsy. Typically the pathologist finds one of the following types of thyroid cancer.
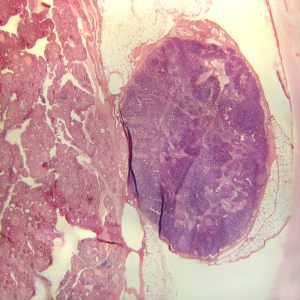
Papillary Thyroid Cancer
This is the most common thyroid tumor that the physician finds at the time of surgical removal. About 75% are of this histological type; another name for this is papillary thyroid adenocarcinoma. It is usually associated with a less invasive, slower growth behavior, in other words persons affected with such a tumor can almost experience a normal life expectancy.
The majority of this type (90%) are variants with a good prognosis. They are the micropapillary, encapsulated, solid and follicular variants. The 5 year survival of this group is 95%, the 10 year survival is 85%. However, an important other 10% of this group is associated with a poor prognosis and they are the tall cell, the columnar cell and the diffuse sclerosing types. It is these variants, which are often found in the older population. They are more invasive and form metastases by invading neighboring areas, which contain a lot of blood vessels. They metastasize into the lungs and bone thus leading to premature death.
Follicular Cancer
This type of thyroid cancer has a worse survival than the papillary thyroid cancer. About 15% of all cases have this appearance under the microscope. The 5 Year survival with optimal treatment is 80%, the 10 year survival is 65%.
Medullary Thyroid Cancer
About 5% of all thyroid cancers are of this type. This is a special type of tumor as it is a tumor of the C type cells of the thyroid, which produces the hormone calcitonin. Often this type of tumor is associated with a familial genetic type of thyroid cancer. The cure rate is usually good, provided it is found early on in the disease and treated appropriately. 10 year survival used to be 50%, but with early diagnosis and aggressive therapy can be as good as 80 to 90%.
Anaplastic Thyroid Cancer
The remaining 5% of all thyroid cancers belong to this immature cell type cancer. It is a very fast growing cancer, which spreads early on to other organs. The survival rates are dismal with overall survival rates of only 7 months to at the most 2 years from the beginning of the diagnosis. About 35% of these cancers develop out of a papillary thyroid cancer in the elderly, which may be a clone of resistant cancer cells that eventually kill the patient.
Thyroid Nodules And Cancer
The thyroid gland has a tendency to produce nodules (lumps) in one or both lobes. In the US about 4 to 7 % of the population have benign thyroid nodules. This is more common in women than in men. The frequency of nodule development throughout life is very constant and is 0.08% per year. For some reason thyroid cancer seems to develop in these nodules and it does so with a frequency of 10 to 20% of these nodules. When there has been an exposure to radiation (x-rays, atomic energy from the Hiroshima bomb, nuclear accident disaster) this rate can go up to 30 or 40% of cancer in thyroid nodules.
Conclusion
As in other cancers early detection and surgical excision is of the utmost importance. The thyroid gland is easily palpable right under the voice box.The patient can often pick up even a small nodule by self-examination. The key for the patient is to take action after the detection of a thyroid lump as described above. A biopsy is done to show what cell type there is. If it is cancer, then it must be removed. Following removal there must be a proper follow-up at regular intervals to make sure that the cancer does not come back.
References
1. Cancer: Principles&Practice of Oncology. 5th edition, volume 1. Edited by Vincent T. DeVita, Jr. et al. Lippincott-Raven Publ., Philadelphia,PA, 1997. Thyroid tumors.
2. Cancer: Principles &Practice of Oncology, 4th edition, by V.T. De Vita,Jr.,et. al J.B. LippincottCo.,Philadelphia, 1993.Thyroid tumors.
3. CC Cheung et al. J Clin Endocrinol Metab 2001 May;86(5):2187-2190.
4. F Dede et al. Clin Nucl Med 2001 May;26(5):396-399.
5. S Hermann et al. Int J Cancer 2001 Jun 15;92(6):805-811.
6. I Sturm et al. J Clin Oncol 1999 May;17(5):1364-1374.
7. VL Greenberg et al. Thyroid 2001 Apr;11(4):315-325.
8. K Ohta et al. J Clin Endocrinol Metab 2001May;86(5):2170-2177.
9. Conn’s Current Therapy 2004, 56th ed., Copyright © 2004 Elsevier
10. Ferri: Ferri’s Clinical Advisor: Instant Diagnosis and Treatment, 2004 ed., Copyright © 2004 Mosby, Inc