Introduction
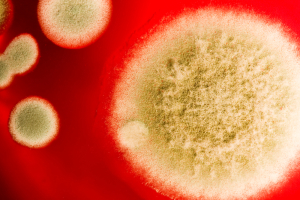
Blastomycosis is a relatively rare disease. Causation is by inhalation of spores of the mold species Blastomyces dermatitidis.
In the US this is found in Ohio in the Mississippi river valleys, in northern Maryland and southern Pennsylvania. In addition, it also occurs in New York (central area), Texas, Florida, southeastern states, northern Midwest and southern Canada. However, there are other areas in the world, such as Africa and the Middle East where the spores are also endemic in the soil.
Conditions for multiplication of this pathogen are particularly good when soil is rich in excretions from animals. Conditions are even better when the soil is acidic and moist containing decaying organic material. Blastomycosis dermatitidis grows at room temperature. When humans inhale the spores and the immune system is weak, conditions are right for blastomycosis to become invasive. The heat increase from room temperature to body temperature (37°C or 98.6°F) also triggers conversion to large invasive yeast bugs.
The lungs immediately attempt to isolate the yeast bugs. Mononuclear white blood cells surround the invading pathogen. In a healthy person that stops the invasion. However, with the weakened immune system inflammatory granulation tissue forms. The disease process enlarges and eventually fibrotic changes and lung scar tissue form. There can also be superinfection with bacteria or other fungal infections such as Candida albicans. Eventually there is an invasion into the circulatory system, which leads to disseminated blastomycosis. Blastomycosis foci are developing in organs such as kidneys, skin, vertebrae and other bones. In addition disseminating blastomycosis affects prostate and testicular tissues, thyroid gland, brain, bone marrow and other tissues. This condition is life threatening and often leads to death.
Symptoms
Usually blastomycosis (also called “Gilchrist’s Disease”) starts as a lung disease. It may not be recognized first and simply present as an infection with chills, a hacking cough and non specific chest pains. The patient may be very tired and have intermittent fevers and sweats. As the physician does a workup he usually orders a chest x-ray. The X-ray finding alerts the physician that his patient presents with something different than the ordinary pneumonia.
Instead of an infiltrate in the periphery of the lung, the infiltrate of blastomycosis fans out from the center of the lung (called”hilum”) into the lung tissue. If the disease is not recognized and it progresses further, the patient gets symptoms from whatever organ is involved in the now disseminated blastomycosis. The most common symptoms are skin lesions that can be more local or often also distributed all over the body surface, but with preference to exposed areas. They look like pimples, but can also look wart like. The lesions heal in the center leaving scarred skin behind, but advancing in the periphery. The advancing border has a steep slope and there are often a number of mini abscesses along this border, which have a purplish red color.
Diagnostic tests
In the earlier form when only lung tissue is involved X-rays show characteristic changes suggestive of blastomycosis. However, bronchoscopy must be done by a respirologist to confirm the diagnosis. Samples can be taken for microscopic slides. The laboratory physician uses special staining techniques that identify blastomycosis. If this is not conclusive, then a blastomycosis cultures confirm the diagnosis, which also detects more minute quantities of the pathogen. Other diseases have to be excluded with appropriate tests such as cancer (bronchogenic carcinoma), mycoses or tuberculosis.
Treatment
If blastomycosis is untreated, it would slowly and relentlessly infect the patient until the patient would succumb to the disease. Mild or moderate disease can be treated very successfully with the antifungal antibiotic itraconazole (brand name: Sporanox). Fluconazole (brand name: Diflucan) is less successful. Patients with severe life threatening infections are treated with intravenous amphotericin B (brand name: Fungizone) (Ref.1, p.1216).
References
1.The Merck Manual, 7th edition, by M. H. Beer s et al., Whitehouse Station, N.J., 1999. Chapter 158.
2.The Merck Manual, 7th edition, by M. H. Beers et al., Whitehouse Station, N.J., 1999. Chapter 113.
3. The Merck Manual, 7th edition, by M. H. Beers et al., Whitehouse Station, N.J., 1999. Chapter 164.
4.David Heymann, MD, Editor: Control of Communicable Diseases Manual, 18th Edition, 2004, American Public Health Association.