Introduction
Syphilis is a sexually transmitted disease that has been around for thousands of years and was for a long time the major venereal disease transmitted through prostitutes. Specifically, the underlying infectious agent is called Treponema pallidum, which is a spiral shaped bacterium.
Certainly, it can be seen utilizing a dark-field microscope. Alternatively a fluorescent technique can be used to demonstrate its presence. In this case it is difficult to culture in a Petri dish in the lab. The spirochetes transmit through intimate skin contact and quickly invade the body via the lymphatic and circulatory systems. There are four characteristic stages.
Primary syphilis
1.The primary stage is the stage of the syphilis lesion. It is a skin sore that enlarges and then breaks open, called “chancre”.
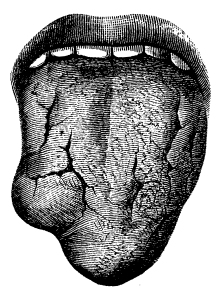
The primary lesions can look quite different depending on the location. This website shows different primary lesions of syphilis. Primary lesions often start as a reddish pimple that clears in the center, but leaks some serum containing lots of syphilis bacteria. Untreated this takes about 4 to 8 weeks to heal. The chancre does not hurt. Another primary lesion on the tongue would look differently. Notably, a neglected primary lesion on a finger has almost a cancer-like look. The regional lymph glands get enlarged, but do not hurt. Characteristic locations of chancre sores are on the penis, the vaginal entrance, the skin between the vagina and the rectum in women (=perineum), and also in the anal and rectal area of homosexual men.
Secondary syphilis
2. The secondary stage of syphilis consists of a skin rash. This is the time when syphilis is blood born and reaches the lymph glands in the whole body, the spleen, the bones, joints, the kidneys, the eyes (called “uveitis”) and the membranes around the brain (syphilitic meningitis). Another key point is that syphilis has been called the “great imitator”, because it can imitate symptoms of many diseases. This can make the diagnosis more difficult. This is because the rash can come in different shades and shapes on the same person and look like eczema, in another person may have a pustular appearance and again in another area look more like plaques.
Involve a dermatologist regarding a syphilis skin rash
The frst thing to remember is that any unknown rash should be looked at by a dermatologist. This specialist knows most about rashes and would not overlook a syphilitic rash. A special form of skin lesions, called condyloma lata, which are soft elevated waxy skin formations with dark pink color, appear on moist skin such as the penis shaft or the labia of a woman. You can use Google to find images regarding the appearance of condyloma lata. In general, they also can occur inside the lips or nose and in the rectal mucosa. Indeed, there are myriads of syphilis bacteria (Treponema pallidum) in the condyloma lata making contact with it very contagious.
Latent stage of syphilis
3. The latent stage of syphilis is an in-between stage where the immune system has contained the infection, but it is still active, just dormant and waiting for the immune system to weaken, so it can flare up. In about 1/3 of untreated latent stage develop the tertiary stage of syphilis. But the majority after several years of the latent stage in development countries will experience a “spontaneous cure”. Truly, this is likely not by chance at all, but due to a fortuitous treatment of a cold with antibiotics, which happen to have covered the patient for syphilis in the latent stage as well.
Tertiary syphilis
4. Tertiary stage of syphilis: This late stage of syphilis is quite varied like a chameleon as it can be a more benign course affecting bone, internal organs and skin. However, it can be more dangerous when if affects the cardiovascular system, such as the aorta or the Central Nervous System (=neurosyphilis).
To point out, the incubation time for tertiary syphilis is about 3 to 10 years from the beginning of the infection. The characteristic lesion for tertiary syphilis is the “gumma”, which consists of central necrotic tissue and a surrounding granulation tissue. As an illustration, histologically gummae are very characteristic of syphilis. In the past (before the modern antibody tests for syphilis) this was the pathological proof to identify the disease.
Gumma lesions
Gumma lesions can develop in all the body organs and lead to scarring and destruction of support tissue. When lesions develop in the aortic wall, the aorta can rupture and the patient may die instantly. In the brain they can cause serious neurological, stroke like symptoms including paranoia. In a bone there might be a sudden pathological fracture and the surgeon may first think it would be a cancerous lesion, but the pathology, cultures and other tests are telling the physician otherwise.
Signs and Symptoms
I described the symptoms largely above and will not repeat it here. In the western world physician prescribe antibiotics frequently for colds, pneumonia, ear infections and urinary infections. For this reason it is rare to see untreated latent stage or tertiary stage syphilis (point 3 and 4 above).
However, it is common that a patient does not have primary or secondary stage syphilis treated and the disease can then spread as explained under point 1 and 2 above. It is therefore important to stress that a physician should examine any skin ulceration or red lesion around the genital area that does not hurt (possibly a chancre).
Doing appropriate tests
The physician has to order appropriate tests as in this stage the pathologist can detect the spirochetes (=the spiral shape Treponema pallidum) with dark-field microscopy. In the secondary stage of syphilis the symptoms can be very misleading. For instance, the joints may show involvement, which means there would be swelling of the joints and symptoms similar to arthritis with joint stiffness and joint pains.
With bone marrow involvement there can be a pronounced anemia, which makes the patient feel fatigued. In addition, the spleen and liver can show enlargement, the appetite may be decreased, the patient feels sick, looses weight and might get jaundice. If meningitis is present, there are headaches, neck stiffness, hearing loss might occur and the eye movements may be abnormal resulting in double vision. When the physician may see edema of the optic nerve (=papilledema) on examination of the eye with an ophthalmoscope.
Seeing a physician in time
The important point to remember is to see a physician and to tell all of these symptoms. The physician examines the patient and orders appropriate blood tests. If a health professional does not do any tests to detect syphilis at this stage, it will relentlessly go on to the latent or the tertiary stage. Gumma can form in the aorta or the brain, possibly killing the patient. Sudden pathological fractures can occur, when syphilis infects the bone and gummas form there. This means that there is a pathological process that softens up the bone and the body’s weight or a force from moving an arm of leg can suddenly lead to a fracture of the bone.
Diagnostic Tests
In primary syphilis the serous discharge from the primary lesion (the chancre) is examined under the dark field microscope and Treponema pallidum can be directly identified. Chancres can also occur outside the genital area and the physician must remember to think about the possibility of syphilis.
Diagnostic evidence of secondary syphilis
Secondary syphilis may be recognized when there is a rash, but this may also be mistaken for other skin rashes. The serological tests for syphilis are usually positive at this stage (a common blood test has the name “VDRL”, which stands for Venereal Disease Research Laboratory). In the latent and in the tertiary stage of syphilis other tests need to be done and it depends somewhat on the clinical presentation. The physician rules out neurosyphilis by lumbar puncture and analysis of the cerebrospinal fluid. The physician orders a bone scan to look for gummas in the skeleton. MRI scans, CT scans and ultrasounds investigations can be useful to look for aortic lesions, cardiovascular syphilis involving heart valves or lesions in the spinal cord or Central Nervous System. The physician will have to individualize the investigations depending on the clinical presentation.
Treatment of Syphilis
For most patients the treatment of choice is penicillin G by injection (except for those allergic to penicillin). They receive 1.2 million units of benzathine penicillin G (brand name: Bicillin LA) intramuscularly into each buttock.
This provides for a good blood level of penicillin G for about 2 weeks. Patients who are allergic to penicillin receive ceftriaxone (brand name: Rocephin) intramuscularly. The dosage of 1 gram every 3 days for 4 doses. Alternatively, the doctor may order erythromycin, tetracycline or doxycycline by mouth. However, there is a big problem with taking the oral medicine regularly and for a complete course of 15 days.
Sexual contacts receive treatments as well
Part of the treatment is to examine and treat all sexual contacts of the syphilis patient. This includes all sexual contacts over the past 12 months as well. There should be no sexual relations until the present partner also receives treatment in order to avoid cross infection. All stages except the tertiary stage receive treatment as outlined above.
In tertiary syphilis the dosages might be higher and the treatment lasts longer. Also, the period of careful follow-up is longer than with the simpler cases.
Treatment of tertiary syphilis
A dosage of 2.4 million units of Bicillin LA in intervals of 7 days for a total of three injections (total of 7.2 million units) is standard for tertiary syphilis. The antibody titres for Treponema pallidum should show a reduction with treatment. There should be at least a 4-fold depletion by 3 months from the treatment start. In the case of neurosyphilis the physician does a lumbar puncture and analysis of the CSF (=cerebrospinal fluid). At the end of the treatment protocol the physician repeats the lumbar puncture. This demonstrates that the therapy has been successful. About 6 to 12 hours after the antibiotic injection half of the patients will have an expected reaction. This has the name Jarish-Herxheimer reaction. It is a generalized reaction to the massive kill of the Treponema pallidum.
The issue of antibiotic-resistant syphilis
In the last 10 years more and more antibiotic-resistant syphilis cases were noted. Azithromycin-resistant strains are very common in Dublin, but also in several US states as this study shows. The reason is that azithromycin is the first line treatment as it is an easy to take oral antibiotic. But benzathine penicillin given into each buttock is still the treatment of choice as no resistance against syphilis has developed yet. However, these injections are somewhat painful.
References
1.The Merck Manual, 7th edition, by M. H. Beers et al., Whitehouse Station, N.J., 1999. Chapter 163.
2.James Chin et al., Editors: Control of Communicable Diseases Manual, 17th edition, 2000, American Public Health Association.
3.The Merck Manual, 7th edition, by M. H. Beers et al., Whitehouse Station, N.J., 1999. Chapter 164.
4. Feldman: Sleisenger & Fordtran’s Gastrointestinal and Liver Disease, 7th ed., © 2002 Elsevier : pages 1306-1307.