Introduction
This is a fungal infection, which affects primarily the lungs, but has become common as progressive disseminated histoplasmosis, particularly in AIDS patients.
It used to be rare in the past decades, but as AIDS has become more common, so has histoplasmosis. Transmission is by Histoplasma capsulatum, which grows in soil as a mold. Dust or soil contaminated with bird or bat droppings is a particularly good breeding ground for Histoplasma capsulatum.
The geographic distribution is similar to blastomycosis as is the growth pattern in soil and the mechanism of changeover from spore to hyphen form inside the lungs, triggered by the rise in temperature from room to body temperature. With confinement of the disease to the lungs, which is a self limiting disease, histoplasmosis often will heal spontaneously, even without antifungal medications. On the other hand, if the progressive disseminated form is developing, the mortality rate without treatment would be in excess of 90%! It is therefore important to diagnose the condition when the outlook is still good and treat it aggressively, if there are signs that it it getting progressive.
Signs and Symptoms
Primary histoplasmosis in the lungs is mostly asymptomatic. The patient may have cold like symptoms, but as it is mostly self limiting like most viruses, the patient may brush this off as nothing when the patient has recovered.
Other patients may develop a fever, cough, fatigue and sometimes pneumonia. If the immune system, particularly the cellular immunity, is weak as it is in AIDS patients or patients with chronic conditions, then more symptoms can occur. This is when the physician should suspect progressive disseminated histoplasmosis. The pathogen spreads from the lungs via the bloodstream into vital organs. This only occurs with weakening of the cellular immune system due to AIDS, cancer, chemotherapy or other debilitating disease (diabetes, end stage pulmonary disease, kidney failure etc.). The pathogen can infect the spleen, lymph glands, kidneys and bone marrow. The pathogens also multiply in the white blood cells (with the name of monocytes, granulocytes and macrophages) that attempt to fight the disease. However, the pathogens overcome the white blood cells.
Skin lesions
Skin lesions can suddenly occur, lesions in the oral cavity, which can get ulcerated and in the gastrointestinal tract that lead to further weakening of the immune system ; this may cause internal bacterial superinfection and subsequent sepsis. Patients are fatigued, in HIV patients their overall condition may be worsening, but histoplasmosis, unless thought of, might be overlooked.
Sudden acute emergencies
It is when suddenly acute emergencies occur that it becomes apparent that this condition is present such as acute blindness on one eye from histoplasma infection of the eye socket, which got there via the bloodstream. Or there might be a sudden worsening of the previously low grade lung infection as a cough is suddenly worsening and x-rays show a chronic cavitary histoplasmosis, which resembles tuberculosis, but bronchoscopy by a respirologist proves the diagnosis on biopsy. Other complications are liver involvement where an inflammatory reactions leads to granulomas. Most of the time these will heal with calcifications that can be seen on imaging tests. Finally, in late progressive disseminated histoplasmosis there can be pleural effusions in the lung cavities, which were caused by spread via the bloodstream.
Diagnostic tests
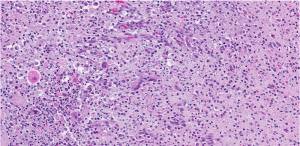
Various body fluids (serum, urine, secretions from phlegm) and biopsy materials(bone marrow, liver, oral ulcerations) can be sent for cultures. Histopathology studies using special fungal stains can also help directly identify Histoplasma capsulatum. For research purposes there is an antigen test available, but this is not readily available in your neighborhood lab.
Treatment
The physician can observe the primary lung form of histoplasmosis without treatment to see whether it resolves spontaneously. However, it may be apparent that the condition turns chronic and is still localized. In this case it may be wiser of the physician to treat it and eradicate it. This is particularly so, if it is in a patient with a known chronic underlying condition that weakens the immune system. Physicians treat mild disease with itraconazole (brand name: Sporanox).
More serious disease such as cavitary histoplasmosis has to be treated with amphotericin B intravenously. This is also the treatment of choice for severe disseminated histoplasmosis (Ref. 1, p. 1214). In AIDS patients the doctor prescribes itraconazole indefinitely for prevention of a relapse. If the patient does not tolerate this, the doctor may order intermittent intravenous therapy with amphotericin B.
References
1.The Merck Manual, 7th edition, by M. H. Beer s et al., Whitehouse Station, N.J., 1999. Chapter 158.
2.The Merck Manual, 7th edition, by M. H. Beers et al., Whitehouse Station, N.J., 1999. Chapter 113.
3. The Merck Manual, 7th edition, by M. H. Beers et al., Whitehouse Station, N.J., 1999. Chapter 164.
4.David Heymann, MD, Editor: Control of Communicable Diseases Manual, 18th Edition, 2004, American Public Health Association.