Why is it so important to go through this detailed, lengthy staging of cervical cancer procedure?
As mentioned in other cancer chapters the cancer survival rate is determined by the initial stage of the cancer at the time of the diagnosis.
As we will see later, different stages of cervical cancer have to be treated differently to get the best cancer cure rates. We have also learnt in the past that for instance to miss pelvic or paraaortic lymph gland metastases at the beginning decrease survival chances significantly.
Many patients now have cures when initial radiotherapy is combined with surgery. So, staging involving the above diagnostic tests makes sense. Here is the FIGO classification:
Staging of cancer of cervix (FIGO classification)
Stage: Description:
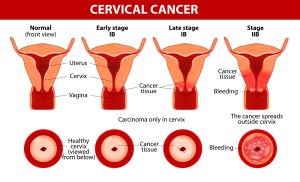
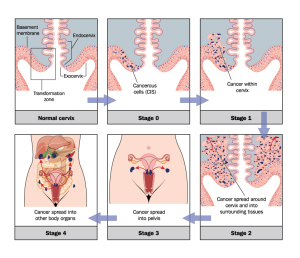
0 : carcinoma in situ
IA : microscopically detectable only ( ‹ 5mm )
IB : tumor invades cervix ( › 5mm )
IIA : Ca.* invades beyond uterus, but not to pelvic wall
IIB : same as IIA, but supportive ligaments are invaded
IIIA : Ca. involves lower third of vagina, but not pelvic wall
IIIB : Ca. extends to pelvic wall, might cause hydronephrosis
IVA : Ca. extends beyond pelvis, or into bladder or rectum
IVB : distant metastases present (e.g. liver, lungs, brain, bone)* Ca. stands for “cancer”
The overall survival figures below under “treatment” are dependent on how far spread the cervical cancer was when it was diagnosed. There is a direct relationship between the invasion of the cancer outside of the cervix and the eventual survival.
The following figure, which is modified from Ref. 1(page 1169 and 1170)and Ref. 2, illustrates this point:
Cervical cancer metastasizing to lymph nodes (LN) along aorta and distant locations
| Stage (FIGO) | LN along aorta (para-aortic LN) | Distant metastases (hematological metastases) |
| IA | 0% | 0% |
| IB | 6% | 5% |
| IIA | 12% | 9% |
| IIB | 19% | 16% |
| IIIA | 24% | 18% |
| IIIB | 29% | 21% |
| IV | 40% | 24% |
This illustration shows that the probability of developing wide spread disease with cancer of the cervix is much higher in later stages than in early stages. Again, this figure also emphasizes how important regular screening methods are for women to catch the dysplastic Pap test changes long before the woman becomes a “statistic” on one of these tables. It also shows that treatment in an earlier stage is much more successful than with later stages.
References
1. Cancer: Principles &Practice of Oncology.4th edition. Edited by Vincent T. DeVita, Jr. et al. Lippincott, Philadelphia,PA, 1993. Chapter on gynecological tumors.
2. Cancer: Principles&Practice of Oncology. 5th edition, volume 1. Edited by Vincent T. DeVita, Jr. et al. Lippincott-Raven Publ., Philadelphia,PA, 1997. Chapter on gynecological tumors.
3. WG Quint et al. J Pathol 2001 May;194(1):51-58.
4. A Duenas-Gonzalez et al. Am J Clin Oncol 2001 Apr;24(2):201-203.
5. BD Kavanagh et al. Am J Clin Oncol 2001 Apr;24(2):113-119.
6. K Nakanishi et al. Skeletal Radiol 2001 Mar;30(3):132-137.
7. M Follen et al. Cancer 2001 May 1;91(9):1758-1776.