Introduction
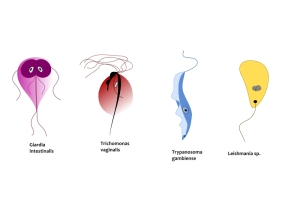
This parasite is distributed worldwide and is transmitted to humans by sandflies from animals like rodents, canines and anteaters.
There are different species of Leishmania that have different body part preferences such as internal organs, skin or the nasopharynx. Here is a brief summary of three common disease entities.
Symptoms and Signs
1. Visceral leishmaniasis
The small bite lesion from the sandfly might go unnoticed. There is an incubation time of a few weeks up to 1 year where the parasite travels via the blood stream or the lymphatic drainage into spleen, liver leading to ascites (thanks to pubs.acs.org for this image), bone marrow and lymph glands. The classical symptom constellation is the combination of undulating fevers, hepatomegaly (large liver) and splenomegaly (large spleen), with low blood cell counts (low red and white blood cell counts, low platelets as well). If this condition is not treated, 90% of patients will die within a period of 1 to 2 years.
Common leishmaniasis subtypes
| Name of disease: | Comments: |
| Visceral leishmaniasis; also known as “kala-azar” or “Dumdum fever” | caused by L. donovani; occurs in India, the Mediterranean, South and Central America, Africa, China |
| Cutaneous leishmaniasis ; also called “oriental sore” or “tropical sore”, “uta ulcer” or “chiclero ulcer”, “Delhi boil” or “Aleppo boil” | caused by L. tropicana and L.major in Asia, Africa and Europe; by L. braziliensis in Central and South America; by L. mexicana in Mexico, Central and South America |
| Mucocutaneous leishmaniasis; also known as “espundia” | caused by L. viannia braziliensis; occurs in Central and South America |
2. Cutaneous leishmaniasis
Within 1 to 4 weeks of the sandfly bite with one of this type of pathogen a skin lesion develops that is sharply demarcated.
This clears in the center as it enlarges and a raised border develops where the parasites are congregated within the skin cells. These skin ulcer (thanks to parasite.org.au for image) are painless, but can get superinfected with bacteria, in which case they become painful. After several months the skin ulcers heal leaving a dimpled scar behind. If there was a mixed infection where L. viannia braziliensis was part of the infection, blood transmitted mucocutaneous lesions in the nose and pharynx can occur.
3. Mucocutaneous Leishmaniasis
A skin lesion develops after the sandfly bite much like in the cutaneous leishmaniasis, but only after an incubation time of 2 or 3 months. This lasts for 1/2 year to just over 1 year. At the same time or only years later, after an asymptomatic interval, relentless ulcerations can occur inside the nose, the palate or the pharynx. The end stage of this are mutilated nasal septa, palates etc.
Diagnostic Tests
There are a number of tests available. The most specific ones involve recombinant antigens and can pinpoint the subtype of Leishmania. There is a leishmanin skin test (also called “Montenegro test”), which turns positive a few weeks to 2 years into the disease, but stays positive for life. Nevertheless this test is useful in the cases of mucocutaneous leishmaniasis, where the disease is not yet broken out in the nasopharynx. Other tests involve blood cultures, cultures of spleen,liver or bone marrow aspirates in the case of visceral leishmaniosis. Finally smears (after special staining) from biopsies of skin or other infected tissue will show the pathogen directly. Interestingly, it is now possible to differentiate between the cutaneous and the mucocutaneous leishmaniosis from skin biopsy material by applying genetic testing using specific DNA probes or alternatively by using monoclonal antibodies.
Treatment
The treatment of this condition should be undertaken by a tropical disease specialist or an infectious disease specialist. Briefly, treatment maybe undertaken with amphotericin B intravenously daily for up to 8 weeks. An alternative is pentamidine isethionate intramuscularly every other day for up to 1 month.
There are older regimens available (e.g. antimony), but there are toxic side-effects like vomiting and the dosage may have to be changed. In some resistant cases of leishmaniasis the reservoir of pathogens in the spleen may have to be removed by doing a splenectomy (=surgical removal of the spleen). Also, treatment with interferon-gamma can be given by infusion. Other general supportive measures such as good nutrition, transfusion in the case of severe anemia, and antibiotic therapy for bacterial superinfections should also be given.
Vaccination is a goal, but this has not been perfected yet, however is under investigation. Kala-azar has been successfully been treated with the newer antifungal antibiotic, itraconazole. This may well become the treatment of choice in future (Ref.6, p.1250).
References
1. The Merck Manual, 7th edition, by M. H. Beers et al., Whitehouse Station, N.J., 1999. Chapter 161.
2. TC Dixon et al. N Engl J Med 1999 Sep 9;341(11):815-826.
3. F Charatan BMJ 2000 Oct 21;321(7267):980.
4. The Merck Manual, 7th edition, by M. H. Beers et al., Whitehouse Station, N.J., 1999. Chapter 43.
5. JR Zunt and CM Marra Neurol Clinics Vol.17, No.4,1999: 675-689.
6. The Merck Manual, 7th edition, by M. H. Beers et al., Whitehouse Station, N.J., 1999. Chapter 162.
7. LE Chapman : Antivir Ther 1999; 4(4): 211-19.
8. HW Cho: Vaccine 1999 Jun 4; 17(20-21): 2569-2575.
9. DO Freedman et al. Med Clinics N. Amer. Vol.83, No 4 (July 1999): 865-883.
10. SP Fisher-Hoch et al. J Virol 2000 Aug; 74(15): 6777-6783.
11. Mandell: Principles and Practice of Infectious Diseases, 5th ed., © 2000 Churchill Livingstone, Inc.
12. Goldman: Cecil Textbook of Medicine, 21st ed., Copyright © 2000 W. B. Saunders Company
13. PE Sax: Infect DisClinics of N America Vol.15, No 2 (June 2001): 433-455.
14. David Heymann, MD, Editor: Control of Communicable Diseases Manual, 18th Edition, 2004, American Public Health Association.