Introduction
Upper gastrointestinal bleeding means that blood is actively shed from the upper digestive tract. In essence, this can either escape upwards (which means vomiting blood), or it can go downwards. That is to say it will be partially digested. And it can reappear as black melena stools. If blood is vomited acutely, this is referred to by physicians as “hematemesis” (“hemat” meaning blood and “emesis” meaning vomiting).
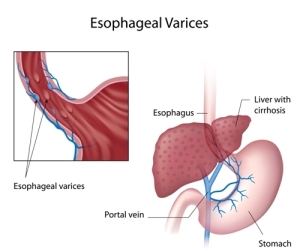
It is important to remember that red blood is a sign there is active bleeding from an artery. In this case, when it has the appearance of “coffee grounds”, it usually means that the bleeding is slower. In essence, there is enough time for gastric juice to alter the red hemoglobin from blood. It changes into the brown colored hematin. Typical causes for hematemesis are: duodenal and gastric erosions and ulcers; esophageal varices (dilated veins) from cirrhosis of the liver. First of all, occasionally there might be a congenital angioma or arteriovenous malformation. These can burst spontaneously. Furthermore, lower gastrointestinal bleed (dealt with under colonic disease) can also confuse the clinical picture.
Symptoms
Ordinarily fresh bleeding is easily visible. In the first place, a nose bleed going direction pharynx can mimic hematemesis. In addition, if bleeding is slow, it appears mostly as melena stools, so the symptoms may be different. Here anemia may be associated with paleness of the skin, sluggishness, shortness of breath and dizziness.
Generally speaking, in an older person significant other diseases are present. For example, they may consist of diabetes, coronary artery disease of the heart, and renal or heart failure. In this case the main symptoms on arrival at the hospital could be the symptoms of a heart attack. This in turn may have been induced by the anemia from the upper gastrointestinal bleed (GI bleed). In other words, the physician faces the challenge of sorting out what is going on while stabilizing the patient’s cardiovascular situation. Regardless, with multiorgan involvement it can be that the patient goes into shock. With this in mind, the shock has to be addressed before anything else can be investigated. Moreover, in less sick patients, the symptoms of the underlying duodenal ulcer might still be present. Indeed, this can give the physician a clue as to the cause of the GI bleed.
Diagnosis
Surely, the doctor will find out with a thorough history whether or not the patient has been taking aspirin or NSAIDs’ for arthritis. Certainly, these drugs break down the mucosal barrier. In addition, some cold medicines may also contain aspirin. Concentrated alcohol can lead to an alcoholic esophagitis or gastritis. However, such a history although important, is not always easy to get. Among other things the doctor is also looking for signs of chronic cirrhosis on physical examination. The next step, therefore, when the patient is stable enough, is for the gastroenterologist to do an emergency panendoscopy in order to detect the source of the upper GI bleed.
Treatment
Notably, general stabilizing measures are important. They include starting two intravenous lines and replacing fluid loss. Likewise, in the case of severe anemia replacement of blood loss through blood transfusions is needed.
Above all, an unconscious patient may have to be intubated to prevent aspiration of vomited material into the lungs. Often the bleeder can be identified with gastroduodenoscopy. Bleeding can be stopped successfully by cauterizing with electrocoagulation. Alternatively, injection of a sclerosing substance or laser treatment will stop the bleeder. At the same time there is a high recurrence rate of bleeding. The introduction of proton pump inhibitors have meant a significant improvement. However, there is still a place for the general surgeon. Above all, when the bleeding cannot be stopped, part of the stomach may have to be removed (partial gastrectomy). Examples are a bleeding gastric ulcer or a bleeding duodenal ulcer. The surgeon may have to use sutures to stop the bleeding.
References
1. M Frevel Aliment Pharmacol Ther 2000 Sep (9): 1151-1157.
2. M Candelli et al. Panminerva Med 2000 Mar 42(1): 55-59.
3. LA Thomas et al. Gastroenterology 2000 Sep 119(3): 806-815.
4. R Tritapepe et al. Panminerva Med 1999 Sep 41(3): 243-246.
5. The Merck Manual, 7th edition, by M. H. Beers et al., Whitehouse Station, N.J., 1999. Chapters 20,23, 26.
6. EJ Simchuk et al. Am J Surg 2000 May 179(5):352-355.
7. G Uomo et al. Ann Ital Chir 2000 Jan/Feb 71(1): 17-21.
8. PG Lankisch et al. Int J Pancreatol 1999 Dec 26(3): 131-136.
9. HB Cook et al. J Gastroenterol Hepatol 2000 Sep 15(9): 1032-1036.
10. W Dickey et al. Am J Gastroenterol 2000 March 95(3): 712-714.
11. M Hummel et al. Diabetologia 2000 Aug 43(8): 1005-1011.
12. DG Bowen et al. Dig Dis Sci 2000 Sep 45(9):1810-1813.
13. The Merck Manual, 7th edition, by M. H. Beers et al., Whitehouse Station, N.J., 1999.Chapter 31, page 311.
14. O Punyabati et al. Indian J Gastroenterol 2000 Jul/Sep 19(3):122-125.
15. S Blomhoff et al. Dig Dis Sci 2000 Jun 45(6): 1160-1165.
16. M Camilleri et al. J Am Geriatr Soc 2000 Sep 48(9):1142-1150.
More references
17. MJ Smith et al. J R Coll Physicians Lond 2000 Sep/Oct 34(5): 448-451.
18. YA Saito et al. Am J Gastroenterol 2000 Oct 95(10): 2816-2824.
19. M Camilleri Am J Med 1999 Nov 107(5A): 27S-32S.
20. CM Prather et al. Gastroenterology 2000 Mar 118(3): 463-468.
21. MJ Farthing : Baillieres Best Pract Res Clin Gastroenterol 1999 Oct 13(3): 461-471.
22. D Heresbach et al. Eur Cytokine Netw 1999 Mar 10(1): 7-15.
23. BE Sands et al. Gastroenterology 1999 Jul 117(1):58-64.
24. B Greenwood-Van Meerveld et al.Lab invest 2000 Aug 80(8):1269-1280.
25. GR Hill et al. Blood 2000 May 1;95(9): 2754-2759.
26. RB Stein et al. Drug Saf 2000 Nov 23(5):429-448.
27. JM Wagner et al. JAMA 1996 Nov 20;276 (19): 1589-1594.
28. James Chin, M.D. Control of Communicable Diseases Manual. 17th ed., American Public Health Association, 2000.
29. The Merck Manual, 7th edition, by M. H. Beers et al., Whitehouse Station, N.J., 1999. Chapter 157, page1181.
30. Textbook of Primary Care Medicine, 3rd ed., Copyright © 2001 Mosby, Inc., pages 976-983: “Chapter 107 – Acute Abdomen and Common Surgical Abdominal Problems”.
31. Marx: Rosen’s Emergency Medicine: Concepts and Clinical Practice, 5th ed., Copyright © 2002 Mosby, Inc. , p. 185:”Abdominal pain”.
32. Feldman: Sleisenger & Fordtran’s Gastrointestinal and Liver Disease, 7th ed., Copyright © 2002 Elsevier, p. 71: “Chapter 4 – Abdominal Pain, Including the Acute Abdomen”.
33. Ferri: Ferri’s Clinical Advisor: Instant Diagnosis and Treatment, 2004 ed., Copyright © 2004 Mosby, Inc.