Introduction regarding Chrohn’s disease
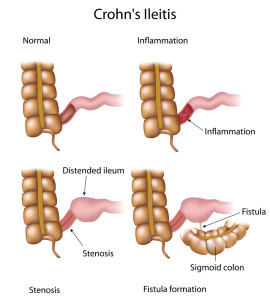
First of all, about 80% of all cases of Crohn’s Disease, an inflammatory bowel disease occur preferentially in the last part of the small bowel (called ileum). Furthermore, 20% develop in the first part of the right sided colon (also called “ascending colon”). The reason that distinction is important is that another inflammatory bowel disease, ulcerative colitis (see below), likes to confine itself solely to the colon and this becomes important for diagnostic purposes.
More detail about Crohn’s disease
There are several distinctions between these two diseases, so proper diagnosis in the beginning is crucial. Crohn’s disease is associated with small ulcerations in the lining of the bowel wall with associated inflammatory changes in the wall, which are called granulomas. On biopsy (small bowel biopsy, colon biopsy) these have a very distinct pathology, which helps for the diagnosis of Crohn’s. Unfortunately these granulomas are also the ones that have given Crohn’s the bad name, as they can melt together leading to complications such as fistula formation or bowel perforation. This in turn is responsible for acute flare-ups of Crohn’s, fistula formation to neighboring bowel loops, the bladder, the rectum, the vagina or the skin.
With the chronic progression of these changes there can be a narrowing of the opening of the bowel eventually leading to a stricture or bowel obstruction. Next, another complication can be an intra-abdominal abscess, when a granuloma perforates the bowel and the bowel contents enter into the abdominal cavity. Crohn’s has a spotty presentation with areas of bowel having been skipped (” skip areas”). To put it differently, this is an important finding on X-rays to support the diagnosis of Crohn’s.
Future more specific anti-inflammatory medication for Crohn’s disease
Lately there are some specific anti-inflammatory treatment modalities that have been developed. The newest classes that have been tested in Crohn’s and ulcerative colitis are the human cytokines (interleukin-11) and the anti-cytokine antibodies (anti-tumor necrosis factor or anti-TNF). Ref. 22-25 deal with interleukin-11. Ref. 26 describes among other medications the use of infliximab, a chimeric antibody targeting the anti-TNF, which has done very well in preliminary clinical trials and early postmarketing experience. However, additional clinical trials are needed to show long-term safety and adverse effects of the medication, but it likely will improve treatment of Crohn’s.
References
- M Frevel Aliment Pharmacol Ther 2000 Sep (9): 1151-1157.
- M Candelli et al. Panminerva Med 2000 Mar 42(1): 55-59.
- LA Thomas et al. Gastroenterology 2000 Sep 119(3): 806-815.
- R Tritapepe et al. Panminerva Med 1999 Sep 41(3): 243-246.
- The Merck Manual, 7th edition, by M. H. Beers et al., Whitehouse Station, N.J., 1999. Chapters 20,23, 26.
- EJ Simchuk et al. Am J Surg 2000 May 179(5):352-355.
- G Uomo et al. Ann Ital Chir 2000 Jan/Feb 71(1): 17-21.
- PG Lankisch et al. Int J Pancreatol 1999 Dec 26(3): 131-136.
- HB Cook et al. J Gastroenterol Hepatol 2000 Sep 15(9): 1032-1036.
- W Dickey et al. Am J Gastroenterol 2000 March 95(3): 712-714.
- M Hummel et al. Diabetologia 2000 Aug 43(8): 1005-1011.
- DG Bowen et al. Dig Dis Sci 2000 Sep 45(9):1810-1813.
- The Merck Manual, 7th edition, by M. H. Beers et al., Whitehouse Station, N.J., 1999.Chapter 31, page 311.
- O Punyabati et al. Indian J Gastroenterol 2000 Jul/Sep 19(3):122-125.
- S Blomhoff et al. Dig Dis Sci 2000 Jun 45(6): 1160-1165.
- M Camilleri et al. J Am Geriatr Soc 2000 Sep 48(9):1142-1150.
- MJ Smith et al. J R Coll Physicians Lond 2000 Sep/Oct 34(5): 448-451.
More references
- YA Saito et al. Am J Gastroenterol 2000 Oct 95(10): 2816-2824.
- M Camilleri Am J Med 1999 Nov 107(5A): 27S-32S.
- CM Prather et al. Gastroenterology 2000 Mar 118(3): 463-468.
- MJ Farthing : Baillieres Best Pract Res Clin Gastroenterol 1999 Oct 13(3): 461-471.
- D Heresbach et al. Eur Cytokine Netw 1999 Mar 10(1): 7-15.
- BE Sands et al. Gastroenterology 1999 Jul 117(1):58-64.
- B Greenwood-Van Meerveld et al.Lab invest 2000 Aug 80(8):1269-1280.
- GR Hill et al. Blood 2000 May 1;95(9): 2754-2759.
- RB Stein et al. Drug Saf 2000 Nov 23(5):429-448.
- JM Wagner et al. JAMA 1996 Nov 20;276 (19): 1589-1594.
- James Chin, M.D. Control of Communicable Diseases Manual. 17th ed., American Public Health Association, 2000.
- The Merck Manual, 7th edition, by M. H. Beers et al., Whitehouse Station, N.J., 1999. Chapter 157, page1181.
- Textbook of Primary Care Medicine, 3rd ed., Copyright © 2001 Mosby, Inc., pages 976-983: “Chapter 107 – Acute Abdomen and Common Surgical Abdominal Problems”.
- Marx: Rosen’s Emergency Medicine: Concepts and Clinical Practice, 5th ed., Copyright © 2002 Mosby, Inc. , p. 185:”Abdominal pain”.
- Feldman: Sleisenger & Fordtran’s Gastrointestinal and Liver Disease, 7th ed., Copyright © 2002 Elsevier, p. 71: “Chapter 4 – Abdominal Pain, Including the Acute Abdomen”.
- Ferri: Ferri’s Clinical Advisor: Instant Diagnosis and Treatment, 2004 ed., Copyright © 2004 Mosby, Inc.