Myelophthisic anemia is a normocytic, normochromic anemia where the bone marrow is wasting away (“phthisis”) secondary to another process.
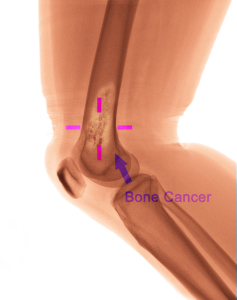
The other process can be a metastasized tumor that displaces bone marrow, or from granulomatous disease (tuberculosis, lupus etc.) or a lipid storage disease. Most commonly the displacement stems from cancers that metastasize into bones, particularly breast cancer and prostate cancer. Others that invade the bone less often are kidney, lung, thyroid and adrenal cancers.
Bone marrow gets displaced
The principle here is that a tumor in the bone or another process in the bone can displace the bone marrow. As a result the precursors of the blood cells including the RBC precursors experience pressure. A primary process of “myelofibrosis” can also occur where fibrous tissue forms in the bone marrow space. Physicians call calcification of this process also “myelosclerosis”. The body can compensate for the loss of bone marrow through a process of “myeloid metaplasia”. This refers to hematopoiesis (production of blood cells) in the liver, the spleen and in lymph glands. A rare genetic cause is Albers-Schoenberg disease. There is osteopetrosis, a calcification of the bones, which leads to fractures.
Symptoms
These are the same as the general symptoms of lassitude, lack of energy and other symptoms described in the introductory chapter to anemia. In addition there are symptoms from the underlying condition. With massive splenomegaly there is abdominal pressure and a feeling of fullness early during a meal. Left upper abdominal pain may be present from abdominal wall muscle spasm. With hepatomegaly there are similar symptoms in the right upper abdomen.
Diagnostic tests
If a normocytic anemia is present in a patient with splenomegaly the suspicion is high for a myelophthisic anemia. A blood smear can determine this further that will show a leuko-erythroblastic pattern (nucleated red blood cells and immature myeloid cells). The morphology of the red blood cells shows high variation, different shapes and sizes. The hematologist can diagnose the condition from these parameters. There is also a low platelet count with giant, bizarre looking platelets. Reticulocytes show elevation due to premature release from the bone marrow and the extra-medullary sites. The final confirmatory test is a bone biopsy, which may be difficult to get, but shows a typical pattern. X-rays of bones may show bony areas from myelosclerosis. There may also be osteoblastic or osteolytic lesions from bone tumors or metastases.
Treatment
The physician treats the underlying condition. In cases where the cause is unknown (so-called “idiopathic form”) the physician provides supportive treatment. This consists of between 20,000 and 40,000 units of erythropoietin. (EPO), given subcutaneously, once or twice per week. The doctor often orders corticosteroids (10mg to 30mg of prednisone daily by mouth). Unfortunately not every patient responds to this. For an enlarged spleen hydroxyurea is given once or every other day (500 mg by mouth). The RBC and spleen normalizing effect of hydroxyurea is very slow; it takes ½ year to 1 year to see results. Thalidomide has an immune modulating effect and can be given as well, but it has serious side-effects (rash, neurotoxicity and high blood pressure).
References
1. Merck Manual (Home edition): Anemia
2. Noble: Textbook of Primary Care Medicine, 3rd ed., Mosby Inc. 2001
3. Goldman: Cecil Medicine, 23rd ed., Saunders 2007: Chapter 162 – APPROACH TO THE ANEMIAS