Introduction
The urethra in the male is part of the ejaculatory tract. Along the urethra there are so-called periurethral glands, which are microscopically small, but are all around the urethra that spans from the level of the bladder to the exit of the urethra. These glands can get infected with a variety of bacteria and viruses, most of which are transmitted sexually from person to person. Common pathogens are: Chlamydia trachomatis, Neisseria gonorrhea and herpes simplex (Ref. 3, p. 1326).
Signs and symptoms
In women the opening of the urethra is in close proximity to the vaginal entrance and inflammatory conditions of the vagina can spill over into the lower end of the urethra.
A woman with a vaginitis from Candida albicans or from Trichomonas vaginalis can experience painful voiding (called”dysuria” in medical terms), which is one of the main symptoms of urethritis.
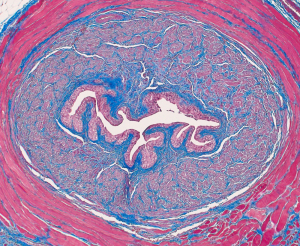
However, associated with these conditions, there is also a discharge from the vagina with a bad odor and painful sex (“dyspareunia”). Sexually transmitted urethritis is usually slower in onset and milder in terms of symptoms. When it produces dysuria, there usually are no vaginal symptoms associated with it. Contrary to a UTI there is usually no blood in the urine. When the urethritis is more established, there is a pussy discharge, dysuria and more frequent voiding. In men the first sign of urethritis might be a discharge from the opening of the urethra at the tip of the penis. This is pussy when it is due to Neisseria gonorrhea, the cause of gonorrhea. If it is due to “non specific urethritis” (meaning it is not due to gonorrhea), it would be a whitish mucous discharge and would mostly reveal Chlamydia trachomatis or else Ureaplasma urealyticum or Mycoplasma genitalium in lab tests (Ref. 3, p.1326). The cross section of the urethra shows many folds where bacteria can hide and multiply.
Diagnostic tests
In the past the only bacterium that could be cultured was Neisseria gonorrhea, the cause of gonorrhea. However, in the last decade newer tests have become commercially available allowing to actually diagnose many of the “non specific” or nongonococcal urethritis cases. More than 50 % of these nowadays are due to Chlamydia trachomatis. The likely reason is the long incubation time of 1 to 4 weeks before persons know that “something is not right” and they see their physician. By that time other partners may have been infected, which makes it difficult from an epidemiological point of view to get a handle on the situation.
The physician can take a swab of the urethral entrance in the male, in the female two swabs are often taken, one from the urethral opening and one from the opening of the cervical canal as Chlamydia trachomatis likes to multiply in that mucous environment. At the present time it is impractical to culture Ureaplasma urealyticum or Mycoplasma genitalium.
With herpes simplex virus infection there are usually several other very painful small skin ulcerations around the genitalia, also in the skin of the labia in women and the skin of the penis in men. A lab test can be sent away and this will identify the virus usually as herpes simplex virus, type 2 (or HSV-2).
Treatment
It is important to determine what the reason for the infection was. This is closely linked to the diagnosis of the underlying pathogen that caused the condition. As mentioned above, in most cases the cause is a sexually transmitted urethritis. Therapy in these cases must be given to the patient and the sexual partner as well to interrupt the infectious chain. In case there were multiple partners involved, these should all be treated, although this is often impossible to do in practice (Ref. 4). The following table has been compiled from data based on Ref. 3 and 4.
___________________________________________________
Therapy of urethritis caused by:
Neisseria gonorrhea : cefixime 400 mg or ciprofloxacin 500 mg orally (both single dose only)
Chlamydia trachomatis : doxycycline 100 mg twice daily for 7 days or azithromycin 1 Gm orally (single dose)
Ureaplasma urealyticum : same treatment as for Chlamydia trachomatis
Mycoplasma genitalium : same treatment as for Chlamydia trachomatis
Herpes simplex, type 2 (HSV-2) : acyclovir 400 mg three times daily for 10 days; or: famciclovir 250 mg three times daily for 5 days; or: valacyclovir 1Gm twice daily for 10 days (all orally)
Candida albicans : fluconazole 200 mg once daily for 5 to 7 days
Trichomonas vaginalis: metronidazole 2 Gm orally as single dose cures 95% of women; in men 500 mg twice per day orally for 7 days
___________________________________________________
Another fact is that sexually transmitted urethritis, like any other form of venereal disease, often involves more than one pathogen: two common combinations are Neisseria gonorrhea and Chlamydia trachomatis as well as Neisseria gonorrhea and Trichomonas vaginalis. This, apart from resistant pathogens, is often the reason for treatment failures. However, with repeat cultures and tests the physician can work this out to the benefit of the patient.
References:
1.The Merck Manual, 7th edition, by M. H. Beers et al., Whitehouse Station, N.J., 1999. Chapter 227.
2.The Merck Manual, 7th edition, by M. H. Beers et al., Whitehouse Station, N.J., 1999. Chapter 261.
3.The Merck Manual, 7th edition, by M. H. Beers et al., Whitehouse Station, N.J., 1999. Chapter 164.
4.James Chin et al., Editors: Control of Communicable Diseases Manual, 17th edition, 2000, American Public Health Association.
5. David Heymann, MD, Editor: Control of Communicable Diseases Manual, 18th Edition, 2004, American Public Health Association.
6. Suzanne Somers: “Breakthrough” Eight Steps to Wellness– Life-altering Secrets from Today’s Cutting-edge Doctors”, Crown Publishers, 2008