The diagnosis of stomach cancer is a diagnosis based on pathology.
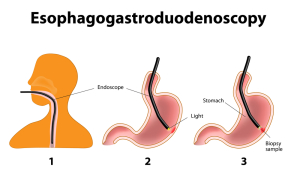
An initial test may be a barium swallow, which shows a shadow of the cancer in the stomach or a distorted anatomy. However, seeing is believing, so the next step after a suspicious X-ray is a gastroscopy to visualize the stomach. With the gastroscope, a fiberoptic instrument, the specialist (gastroenterologist, surgeon or internist) can see the cancer and then take brushings and biopsies.
Here is a link to a picture from such a gastroscopic procedure (arrows point to early stomach cancer).
After analysis of these samples by a pathologist the histology makes the diagnosis of stomach cancer. There are two main types that are found on large series of patients as can be seen from the table.
Histological types of stomach cancer
____________________________
gastric adenocarcinoma : 80 % of all cases
gastric adenocarcinoma : 19% of all cases
rare types (leiomyosarcomas etc.) : 1 % of all cases
____________________________
By far the most common type is the adenocarcinoma. In the last decades pathologists have found a shift from only 3% of lymphoma to 19% of all stomach cancers. Rare other types is the leiomyosarcoma, which originates from the muscle tissue of the stomach; squamous cell carcinoma, which originates from lining similar to the esophagus, and others. It is important to differentiate between these different cellular types as the treatment differs depending on what histological type it is.
The pathologist will also report the grade of the cancer cells, which over the years has been classified into different categories. Broders’ classification distinguishes 4 histological grades, where grade 1 is well differentiated and has a better outcome, and grade 4 is called “anaplastic” grade and is associated with early distant metastases and a very poor outcome (Ref.1, page 822).
The further work-up of the patient with diagnosed histological stomach cancer concentrates on establishing how widespread the cancer is. In other words, the physician needs to know whether the cancer is still confined to the stomach or whether it has spread regionally or even further into the rest of the body. To facilitate this CT scans of the abdomen and chest are ordered to screen for lymph gland metastases and local spread of the cancer. Endoscopic ultrasonography (=EUS, thanks to www.medscape.com for this image) using a high frequency transducer at the end of an endoscope allows highly accurate staging of the stomach cancer (“TU” in this image is where the gastric carcinoma, the tumor, was located). The quality of images using this technique is superior to CT and MRI scanning and localizes lymph gland metastases as well.
References:
1. Cancer: Principles &Practice of Oncology.4th edition. Edited by Vincent T. DeVita, Jr. et al. Lippincott, Philadelphia,PA, 1993. Chapter on Cancer of the stomach.
2. Cancer: Principles&Practice of Oncology. 5th edition, volume 1. Edited by Vincent T. DeVita, Jr. et al. Lippincott-Raven Publ., Philadelphia,PA, 1997. Chapter on Cancer of the stomach.
3. J Sun et al. Eur J Cancer Prev 2001 Feb;10(1):61-67.
4. SS Mirvish et al. Nutr Cancer 1998;31(2):106-110.
5. JM van Maanen et al. Cancer Detect Prev 1998;22(3):204-212.
6. JM van Maanen et al. Environ Health Perspect 1996 May;104(5):522-528.
7. B. Sears: “The age-free zone”.Regan Books, Harper Collins, 2000.
8. B. Sears: “Zone perfect meals in minutes”. Regan Books, Harper Collins, 1997.
9. K Murakami et al. Am J Clin Pathol 2001 Feb;115(2):224-34.
10. Y Tsubono et al. N Engl J Med 2001 Mar 1;344(9):632-636.
11. Conn’s Current Therapy 2004, 56th ed., Copyright © 2004 Elsevier
12. Ferri: Ferri’s Clinical Advisor: Instant Diagnosis and Treatment, 2004 ed., Copyright © 2004 Mosby, Inc