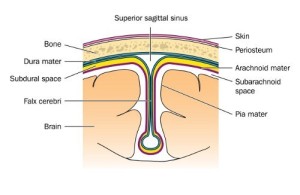
Dementia due to subdural hematoma can develop following head trauma with a disruption of subdural veins and slow leakage of blood, which can accumulate.
With an acute subdural hemorrhage (thanks to www.nlm.nih.gov for this image) the patient is usually seen fairly rapidly by a neurosurgeon as the symptoms are acute and lead to unconsciousness.
An MRI scan or CT scan will usually show the problem and the neurosurgeon will attempt to repair it. However, with a chronic subdural hematoma there is often a 2 to 4 week interval between the head trauma and the onset of symptoms and the patient may be an alcoholic who does not remember a closed head injury from a fight or a fall on a staircase.
The symptoms of a subdural hematoma are constant headaches, drowsiness and mental confusion that might come and go, but overall there is a deterioration of the neurological functioning. However, there might be some gait problem and diminished upper extremity function suggesting a partial hemiparesis alongside the increasing confusion.
The patient affected with a subdural hematoma depends on a family member or friend to bring this to the attention of the medical profession. If left alone, such a patient would stay in a demented state due to the pressure from the subdural hematoma leading to permanent pressure atrophy of at least part of the brain.
However, if at the 2 to 4 week point the patient is brought to the attention of a neurosurgeon, a CT or MRI scan would depict the problem, the subdural hematoma would be evacuated through neurosurgery and the patient would very likely have a good chance to recover and function normally in a high percentage of cases. If the subdural hematoma has been in place for 1 year or longer surgery likely will not help any more because of permanent damage to the adjacent brain tissue.
References:
1. OL Lopez et al. Neurology 2000 Dec 55(12):1863-1869.
2. K Yasojima et al. Brain Res 2000 DEC 887(1):80-89.
3. A Kontush et al. FreeRadicBiol Med2001Jan30(1): 119-128.
4. H Vanderstichele et al. Amyloid 2000Dec7(4):245-258.
5. Neely et al. Lipids 2000 Nov35(11):1249-1257.
6. RA Yokel Neurotoxicology 2000 Oct21(5):813-828.
7. Petanceska et al. Exp Gerontol 2000 Dec 35 (9-10):1317-1325.
8. MB Liddell et al. Brit J Psychiatry 2001 Jan 178: 7-11.
9. Sramek et al.ExpertOpinInvestigDrugs2000Apr9(4):899-915.
10.K Kosaka et al. Neuropathology 2000 March 20(1): 1-7.
11.V Haroutunian et al.Arch Neurol 2000 Aug57(8):1145-1150.
12. C Puckett et al. Am J Hum Genet 1991Aug49(2):320-329.
13. M Haltia Ann Med 2000 Oct 32(7): 439-500.
14. Ferri: Ferri’s Clinical Advisor: Instant Diagnosis and Treatment, 2004 ed., Copyright © 2004 Mosby, Inc.
15. Rakel: Conn’s Current Therapy 2004, 56th ed., Copyright © 2004 Elsevier