Introduction
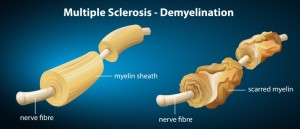
Multiple sclerosis is a slowly progressing neurological disease, which affects the central nervous system. There are patches of demyelination where the myelin sheath, which functions similar as insulation material around electric wires does, breaks down in a process called demyelination.
For electrical signals that were generated in the brain to safely arrive at any part in the body, intact “wires” are needed to deliver the message. In the nervous system of the body these “wires” are called nerve tracts. They are made up of nerve fibers in the center of the tract and they are surrounded by insulation material, which is made up of living cells such as the oligodendroglia cells and Schwann cells.
They stretch out thin tentacles that wrap around the nerve fibers. This way they form an insulation layer and enhance the speed of nerve impulse transmission.
With multiple sclerosis demyelination foci can be seen in the brain and the spinal cord using MRI scanning technology.
On a histological level there is a breakdown of these insulating cells that provide the tentacles that normally wrap around the nerve fibers. Inflammation develops around these foci of demyelination, which eventually leads to scarring. In the beginning the nerve cells and the axon fibers are preserved. However, in the later stages of multiple sclerosis nerve fibers are also destroyed, particularly in the long tracts of the spinal cord, and are replaced with “fibrous gliosis”, which is just another term for scar tissue. These can be distinguished on an MRI scan as “old lesions”. “New lesions” from an early inflammatory reaction have a different appearance on the MRI scan.
Causes of MS
At this point the cause for multiple sclerosis is not known. However, we do know that there is an immunological abnormality taking place at the level where these demyelination foci occur. For many years it has been postulated that certain neurotropic viruses such as red measles, human herpes virus or retroviruses may after an initial infection go “underground” and incubate within nerve cells. A secondary immune response some 15 years later would then be the cause of the initial multiple sclerosis attack. It is postulated that there are certain HLA cell surface antigen constellations that are associated with a higher risk for multiple sclerosis. This line of work was initiated when pockets of families with a higher incidence of multiple sclerosis were found. A certain HLA constellation was found to lead to a higher genetic susceptibility.
Lack of vitamin D3
Other factors are certain geographic factors. For instance, it was noted that multiple sclerosis is more common in temperate climatic regions where the incidence is 1 case in 2,000 of the population. In the tropics the incidence is only 1 in 10,000, fivefold less. Another interesting observation is that this high frequency versus low frequency occurrence of multiple sclerosis has been linked to the geographic area (thanks to www.sunarc.org for this link) where the first 15 years of a person’s life were spent. The onset of the first multiple sclerosis symptoms are typically in the age range of 20 to 40 years. Women tend to get it more often than men. Full spectrum sunlight (the natural light from the sun) produces vitamin D in the skin. Lately it has become clear that much higher doses of vitamin D3 should be taken as a supplement (average of 4000 to 5000 IU per day). Some people are very poor absorbers who may need even higher doses. Vitamin D3 is very safe and toxic levels have so-far not been detected. The best is to measure the 25-hydroxy vitamin D level in the blood.
MS as autoimmune disease
The above notion of MS being an autoimmune disease is getting more and more confirmed by newer research and new therapies that have been recently developed or trials that are still ongoing, but very promising. This was reviewed at the 50th Annual continuing education conference of St. Paul’s in Vancouver/BC/Canada by Dr. John Hooge, Director of the UBC MS Clinic (Ref. 6). It is now confirmed that there are two steps for MS before it becomes irreversible: First there is the inflammatory phase of early MS where the autoimmune antibodies cause inflammation and loss of the nerve pathways, seen on MRI scans as lesions. Secondly, with the later MS there is further deterioration of the nerve pathway lesions by a degenerative process that leads to the final destruction and interruption of the nerve pathways, but there is little inflammation and therefore little change on the MRI scans.
A Canadian trial involving 24 patients is on the way at the present time where the immune system was inactivated with high doses of chemotherapy and the patients’ own bone marrows that were harvested prior to the chemotherapy were re-injected into the patients to re-establish a healthy immune system without the autoantibody-producing immune cells. Some of these patients have experienced miraculous turnarounds of their MS, but there is a 10% mortality associated with the bone marrow transplant and longterm studies have to be awaited as to whether the initial encouraging results hold true. There is also a late complication from high doses of chemotherapy with leukemias being more common 5 to 10 years down the road.
Genetic tests with experimental animals (autoimmune mouse model) have shown encouraging results, but to translate these successes safely into the human situation can take many years, if not decades.
There are other attempts to solve the multiple sclerosis puzzle. This web site about a surgical approach for multiple sclerosis (thanks to www.cbc.ca for this link) by Dr Zamboni and others shows that a lot is still unknown about the causes of this illness.
Chronic Inflammation and MS
There is an agreement that MS is a chronic inflammatory condition of the central nervous system (see Ref. 7). All of the various possible causes are not entirely clear at this moment. However, it seems that certain foods can cause MS, such as a lack of vitamin D3 and the intake of too much saturated fat (see Ref. 8). In other words dysbalanced food intake with too much sugar and starch and a lack of vegetables and too much saturated fat (lack of omega-3 fatty acids) can lead to changes in the immune system and the setting up of chronic inflammation. It follows from this that attention to proper nutrition and the taking of vitamins and supplements likely is useful for MS patients. Even coffee consumption, which has anti-inflammatory effects has ben shown to be useful.
References:
1. Z Liu et al. J Neuroimmunol 2001 Jan 1;112(1-2): 153-162.
2. C Liu et al J Neurol Sci 2000 Dec. 1; 181(1-2): 33-37.
3. The Merck Manual: Multiple sclerosis (thanks to www.merckmanuals.com for this link)
4. Ferri: Ferri’s Clinical Advisor: Instant Diagnosis and Treatment, 2004 ed., Copyright © 2004 Mosby, Inc.
5. Rakel: Conn’s Current Therapy 2004, 56th ed., Copyright © 2004 Elsevier
6. The 50th Annual St. Paul’s Hospital Continuing Medical Education Conference for Primary Physicians, Nov. 16 – 19, 2004
7.http://www.clevelandclinicmeded.com/medicalpubs/diseasemanagement/neurology/multiple_sclerosis/
8.http://www.nutritionmd.org/health_care_providers/neurology/ms_nutrition.html