There are a number of potential complications of ulcerative colitis (UC) that the physician needs to be attend to right away to avoid life threatening situations. I am discussing six of the more common complications here.
1. Toxic Colitis
First, the ulcerations usually are quite superficial with ulcerative colitis. However, in some patients there is a sudden deterioration and the pathological inflammatory process decides to extend deeper into the colon wall and beyond. This results in paralysis of the affected bowel section, called paralytic ileus. It also leads to leakage of E.coli bacteria and other gut flora into the abdominal cavity, which in turn causes peritonitis.
These conditions are very serious and have a high death rate even with treatment. X-rays show the ileus as dilated bowel loops with gas and fluid levels in it. Because of a lack of bowel propulsion in this segment, it functions like a block and nothing will move through the gut. The patients look sick, have a high fever and vomit. Peritonitis leads to severe abdominal pain and a high fever and there is a rigid abdomen. The surgeon seeing the patient with an underlying bowel perforation is ordering intravenous antibiotics. Whenever the patient is stable enough, the surgeon will do a laparotomy to attend to the internal problems.
2. Massive Rectal Hemorrhage
Second, although bleeding is normally part of the clinical presentation of UC, in a minority of patients there is a sudden deterioration with profuse blood coming out with every bowel movement and the bowel movements are getting more and more frequent. This is an emergency situation as the patient could bleed to death, if left alone.
In this case a general surgeon needs to see the patient on an emergency basis. He/she will likely do a partial removal of the bleeding colon (called “subtotal colectomy”). The surgeon then makes an artificial opening for the cut ileum through the abdominal wall (called ” ileostomy”). Subsequently the surgeon closes the rectosigmoid stump at that time.
Recovery of the patient
Most patients tolerate this emergency procedure. The patient usually improves dramatically. The rectal bleeding now stops and the nutritional status improves as well. In the future, the patient can undergo further surgery on an elective basis when the patient’s state is more stable. This consists of removal of the rectosigmoid portion left behind; otherwise ulcerative colitis could recur in that portion of the large intestine. At the same time the surgeon fashions an intestinal pouch out of ileus tissue. In this case the surgeon can transfer this into the pelvic area and replace the lost rectum. The surgeon completes the procedure by connecting the intestinal pouch with the anus (called “ileoanal anastomosis”). The intestinal pouch serves as a reservoir for stool, which cuts down on the amount of stools per day and makes the stools more formed.
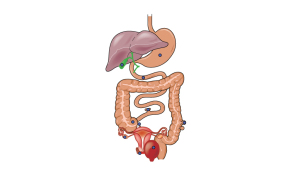
Complications Of Ulcerative Colitis (Perforated UC Is Only One Of The Causes Of Perforation causing Peritonitis)
3. Acute Perforation
Third, another complication that is life threatening is when one of the ulcers of the large intestine perforates. As the disease is usually most severe in the sigmoid colon area, this likely will be the area where one of the deep ulcers perforates. This is an emergency, because bowel contents with lots of E.coli and other bacteria flow freely into the abdominal cavity. The general surgeon needs to do open the abdomen (do a” laparotomy”) and look for the area of perforation. The surgeon likely will do the same procedure as described under point 2 above (emergency “subtotal colectomy“). Once ulcerative colitis has progressed to such a point that there is perforation, the chances that this will happen again soon in another diseased location are very high. It makes therefore sense to do what appears to be a rather invasive procedure.
4. Cancerous Degeneration
Furthermore, after ulcerative colitis has been symptomatic in a patient for more than 10 years, a significant number of patients show dysplasia (the immediate stage before cancer) and some frank colonic cancers on colonoscopy with biopsies. The longer the patient has ulcerative colitis, the higher the chance of developing colon cancer in the chronically irritated mucosa of the colon.
For this reason, any patient who has ulcerative colitis for more than 8 years should have regular colonoscopies (endoscopic examinations with a fiberoptic instrument) through a gastroenterologist. This will allow to screen for mucosal dysplasia. Once the doctor diagnoses mucosal dysplasia for the first time, the patient requires an elective total colectomy. The mucosal dysplasia shows a deterioration of the ulcerative colitis.
Total colectomy for mucosal dysplasia in colon
This means there will be cancer in the very near future. Often at the time of surgery, there is already early cancer in another area. The colonoscopy likely has missed this in the past. This is an emotional topic, but the patient needs to understand that total colectomy is presently the only alternative to dying later of colon cancer. After a total colectomy the patient has a normal life expectancy. In the past these patients had to accept living with an ileostomy (changing pouches etc.). Now there is an alternative with doing an ileoanal anastomosis using an intestinal pouch, in which case there are normal bowel movements and no more risk of a recurrence of ulcerative colitis. This is so, because ulcerative colitis never goes beyond the limit of the colon.
5. Primary Sclerosing Cholangitis
Another complication is primary sclerosing cholangitis. In about 5% of patients with ulcerative colitis a severe obstructive form of cholangitis (primary sclerosing cholangitis) develops in the bile ducts of the liver and the bile ducts. This leads to jaundice and a chronic skin itch.
The physician can arrange for an ERCP (endoscopic retrograde cholangiopancreatography) to visualize the strictures in the bile ducts. The gastroenterologist will attempt to localize a stricture and possibly place a stent to overbridge it. But each case is different. The longer the patient has had ulcerative colitis or Crohn’s disease, the higher the danger of this complication. Unfortunately, there is also a high incident of cancer in the bile ducts (“cholangiocarcinoma”) that develops in these patients. There is a link between Crohn’s, ulcerative colitis and primary sclerosing cholangitis. This likely is due to severe changes in the immune system. Researchers describe autoimmune phenomena both in terms of autoimmune antibodies as well as autoimmune T lymphocytes. More research is necessary in this area before new less invasive therapies will be available.
6. Other complications
Finally, a group of patients, often associated with the cell surface antigen HLA-B27, have arthritis of the major joints, lower back pain (due to ankylosing spondylitis and sacroiliitis) and growth retardation in children. Other potentially dangerous conditions are recurrent inflammatory eye conditions (episcleritis and uveitis). The patient needs to see an eye specialist on an urgent basis for appropriate treatment. Often symptoms of these conditions can precede ulcerative colitis by many years.
References
1. M Frevel Aliment Pharmacol Ther 2000 Sep (9): 1151-1157.
2. M Candelli et al. Panminerva Med 2000 Mar 42(1): 55-59.
3. LA Thomas et al. Gastroenterology 2000 Sep 119(3): 806-815.
4. R Tritapepe et al. Panminerva Med 1999 Sep 41(3): 243-246.
5. The Merck Manual, 7th edition, by M. H. Beers et al., Whitehouse Station, N.J., 1999. Chapters 20,23, 26.
6. EJ Simchuk et al. Am J Surg 2000 May 179(5):352-355.
7. G Uomo et al. Ann Ital Chir 2000 Jan/Feb 71(1): 17-21.
8. PG Lankisch et al. Int J Pancreatol 1999 Dec 26(3): 131-136.
9. HB Cook et al. J Gastroenterol Hepatol 2000 Sep 15(9): 1032-1036.
10. W Dickey et al. Am J Gastroenterol 2000 March 95(3): 712-714.
11. M Hummel et al. Diabetologia 2000 Aug 43(8): 1005-1011.
12. DG Bowen et al. Dig Dis Sci 2000 Sep 45(9):1810-1813.
13. The Merck Manual, 7th edition, by M. H. Beers et al., Whitehouse Station, N.J., 1999.Chapter 31, page 311.
14. O Punyabati et al. Indian J Gastroenterol 2000 Jul/Sep 19(3):122-125.
15. S Blomhoff et al. Dig Dis Sci 2000 Jun 45(6): 1160-1165.
16. M Camilleri et al. J Am Geriatr Soc 2000 Sep 48(9):1142-1150.
More references
17. MJ Smith et al. J R Coll Physicians Lond 2000 Sep/Oct 34(5): 448-451.
18. YA Saito et al. Am J Gastroenterol 2000 Oct 95(10): 2816-2824.
19. M Camilleri Am J Med 1999 Nov 107(5A): 27S-32S.
20. CM Prather et al. Gastroenterology 2000 Mar 118(3): 463-468.
21. MJ Farthing : Baillieres Best Pract Res Clin Gastroenterol 1999 Oct 13(3): 461-471.
22. D Heresbach et al. Eur Cytokine Netw 1999 Mar 10(1): 7-15.
23. BE Sands et al. Gastroenterology 1999 Jul 117(1):58-64.
24. B Greenwood-Van Meerveld et al.Lab invest 2000 Aug 80(8):1269-1280.
25. GR Hill et al. Blood 2000 May 1;95(9): 2754-2759.
26. RB Stein et al. Drug Saf 2000 Nov 23(5):429-448.
27. JM Wagner et al. JAMA 1996 Nov 20;276 (19): 1589-1594.
28. James Chin, M.D. Control of Communicable Diseases Manual. 17th ed., American Public Health Association, 2000.
29. The Merck Manual, 7th edition, by M. H. Beers et al., Whitehouse Station, N.J., 1999. Chapter 157, page1181.
30. Textbook of Primary Care Medicine, 3rd ed., Copyright © 2001 Mosby, Inc., pages 976-983: “Chapter 107 – Acute Abdomen and Common Surgical Abdominal Problems”.
31. Marx: Rosen’s Emergency Medicine: Concepts and Clinical Practice, 5th ed., Copyright © 2002 Mosby, Inc. , p. 185:”Abdominal pain”.
32. Feldman: Sleisenger & Fordtran’s Gastrointestinal and Liver Disease, 7th ed., Copyright © 2002 Elsevier, p. 71: “Chapter 4 – Abdominal Pain, Including the Acute Abdomen”.
33. Ferri: Ferri’s Clinical Advisor: Instant Diagnosis and Treatment, 2004 ed., Copyright © 2004 Mosby, Inc.
34. Rakel: Conn’s Current Therapy 2004, 56th ed., Copyright © 2004 Elsevier






