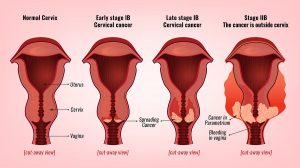
It is possible to approach cancer of the cervix in the early stages with minimally invasive cervical cancer surgery. Today about 60% of women receive this type of treatment. In the past, before laparoscopic radical hysterectomy was available, the traditional radical hysterectomy was done as an open procedure.
The results of two studies are in the New England Journal of Medicine to compare the risk of dying after these two procedures.
The studies compared survivor statistics for early cancer of the cervix, but with two different surgical procedures. The one was the minimally invasive radical hysterectomy as a laparoscopic procedure, the other the traditional open radical hysterectomy.
Details about the study
About half of 2,461 early stage cervical cancer patients received two types of surgery. Either a minimal invasive radical surgery was used to treat their cancer; the other half had an open radical hysterectomy. The researchers followed their patients for 4 years and calculated their survival data. 94 patients from the minimally invasive group died in the first 4 years. This translated into a risk of 9.1% of dying. 70 patients of the open surgery group died in the first 4 years following surgery, which was a 5.3% risk of death.
Minimally invasive, radical hysterectomies are a standard procedure on a large scale since 2006. The researchers noted that the mortality of patients who underwent minimally invasive radical hysterectomies showed a drop in survival rates since 2006 by 0.8% every year.
Second study comparing minimally invasive surgery with open, radical hysterectomy
Another group did a similar study comparing minimally invasive surgery with open, radical hysterectomies. 319 patients received minimally invasive surgery and 312 received treatment with open surgery (traditional hysterectomies). Among the minimally invasive group 84.4% underwent laparoscopy and 15.6% had robot-assisted surgery. The average age of the patients was 46 years. All of the patients in both groups had early stage cancer. Here were the findings.
Details about survival with minimally invasive surgery versus open surgery
- The disease-free survival at 4.5 years following surgery was 86.0% for the group with minimally invasive surgery and 96.5% for the group with open surgery. In other words, there was a survival advantage for traditional open hysterectomy over 4.5 years of 10.5%!
- Minimally invasive surgery had a 91.2% disease-free survival rate at 3 years. This compared to 97.1% at 3 years for the open surgery. The hazard ratio for disease recurrence or death from cervical cancer for the minimally invasive surgery was 3.74-fold compared to the open surgery.
Conclusion
The authors of these studies showed that the outcome was much better among patients who had the traditional open radical hysterectomy with removal of pelvic lymph nodes. Over 4.5 years there was a 10.5% survival advantage with traditional open radical hysterectomies. These are facts that women with early cervical cancer should know. They should discuss this with their physician and specialist. There may be less intraoperative blood loss for the minimally invasive procedures. The newer methods have a shorter hospital stay and less postoperative complications. However, the long-term survival rates are in favor of the traditional open radical hysterectomy. It clearly shows a longer disease-free survival rate, the rate of recurrence is lower, and the overall survival rate is longer than the statistics for the minimally invasive surgery. Sometimes newer methods seem to appear more promising, but in this case the traditional method wins giving the patient a better chance!