It is important to realize that the clinician makes the diagnosis of fibromyalgia clinically by the history and certain physical findings as mentioned above. At the same time it is done by exclusion of other rheumatic conditions that may produce fibromyalgia symptoms very similar to other conditions as mentioned above in the introduction.
In fact, very often it is a young or middle-aged woman who is first diagnosed with this condition.
In like manner, in older women it often is associated with a minor osteoarthritic condition, which is not associated with the fibromyalgia, but which in some way seems to contribute or worsen the fibromyalgia. On the other hand, in men fibromyalgia often follows a work related injury or a sports injury and may develop out of a “myofascial pain syndrome” in association with such an event (Ref.3, p. 481).
Fibromyalgia is a multifactorial entity
By the same token the various reference materials seem to agree that there is no single cause for fibromyalgia. On the contrary, it likely will ultimately be found that it is a multifactorial, but very real entity. In like manner a contributing factor can be a physician with a closed mind who makes a statement to a patient with fibromyalgia like “it is all in your head”. Such a physician, instead, would do better referring the patient to a rheumatologist. What this uncaring statement really is communicating is the frustration that the physician feels: the aching muscles and other persistent symptoms did not respond to the usual anti-inflammatory interventions that, for instance, arthritis cases respond to. However, fibromyalgia is a condition that is known not to be due to inflammation, for this reason anti-inflammatories will not tend to help that much.
Sleep laboratory and blood tests
For example, a fibromyalgia patient with a lot of sleep disturbance should be send to a sleep laboratory, which likely will document a certain type of sleep disorder that can be treated accordingly. Moreover, the physician orders a number of blood tests to rule out hypothyroidism (TSH level), rheumatoid arthritis(RA titre) and lupus (ANA titre). In addition, a blood sugar or a hemoglobin A1C level would be useful to rule out diabetes. Depending on what the physician detects during the physical examination other tests may also be done. In a study researchers examined people with acute chest pain and did coronary artery angiograms (X-rays of the coronary arteries). These showed that less than 30% of the patients had actual narrowing of the coronary arteries (actual angina chest pain).
Costochondritis and fibromyalgia
Of the patients who had normal coronary arteries 30% were due to fibromyalgia and 10% due to costochondritis (an inflammatory disease of the junction between a rib and the chest bone). In contrast, the group with coronary artery disease had only 2.5% of fibromyalgia and no costochondritis (Ref.5). In short, the authors concluded that patients with chest pain and normal coronary arteries often have a number of rheumatic diseases with the most common one being fibromyalgia.
A point often overlooked, but very important comes from the anti-aging medicine approach. It is to do a saliva hormone panel as often the hormone levels of progesterone, testosterone or DHEAS are low with fibromyalgia patients (Ref. 8). It must be remembered that when low hormone levels are found, the quickest way to help a fibromyalgia patient is to administer the missing hormones.
Factors found in fibromyalgia
________________________________________________
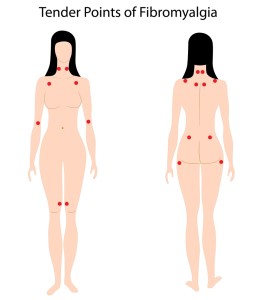
– muscles, ligaments and tendons ache : 12 out of 18 fibromyalgia tender spots or more are positive
– sleep disorders : can be verified by sleep studies in a sleep laboratory
– moderate depression : often present, likely due to a change in serotonin metabolism
– rule out other medical and rheumatological diseases : blood tests help in that regard (RA, ANA titres normal; TSH and Hgb A1C normal)
– precipitating factors often present : trauma, degenerative arthritis, emotional stress
– patients with chest pain : if coronary arteries normal and cardiovascular disease is excluded, fibromyalgia is often the diagnosis
– hormone deficiency : hormone testing may show low progesterone, testosterone, DHEAS, cortisol; blood tests may show low IGF-1, indicating low human growth hormone
________________________________________________
References
1. G.Littlejohn Aust Fam Physician 2001 Apr;30(4):327-333.
2. LS Brecher et al. J Am Osteopath Assoc 2001 Apr;101(4 Suppl Pt 2):S12-17.
3. The Merck Manual, 7th edition, by M. H. Beers et al., Whitehouse Station, N.J., 1999. Chapter 59.
4. ABC of rheumatology, second edition, edited by Michael L. Snaith , M.D., BMJ Books, 1999. Chapter 6. Fibromyalgia Syndrome.
5. B Mukerji et al. Angiology 1995 May;46(5):425-430.
6. Ferri: Ferri’s Clinical Advisor: Instant Diagnosis and Treatment, 2004 ed., Copyright © 2004 Mosby, Inc.
7. Rakel: Conn’s Current Therapy 2004, 56th ed., Copyright © 2004 Elsevier
8. Dr. Edward M. Lichten: Textbook of bio-identical hormones. © 2007 Foundation for Anti-Aging Research, Birmingham, Michigan, USA