It is important to realize that unfortunately at this point in time treatment for Crohn’s disease is not a cure. Certainly, Crohn’s belongs to the diseases, which can not be cured, but can only be controlled. In essence, sulfosalazine (brand names: Salazopyrin, Azulfidine) is a medication, which has improved management of Crohn’s disease tremendously. It has anti-inflammatory effects and is useful in mild to moderate cases of Crohn’s to tone down the amount of inflammation. Frequently it also maintains remissions for longer.
The main metabolite is mesalamine or 5-amino-salicylic acid (brand names: Rowasa, Asacol, Mesasal, Pentasa, Quintasa and Salofalk), which is especially useful for those patients who are allergic to Salazopyrin. 5-amino-salicylic acid has been shown to prevent recurrence of Crohn’s disease following surgery. In addition, 5-amino-salicylic acid can induce and maintain remissions of acute flare-ups of Crohn’s.
Use of corticosteroids
All of a sudden the physician may need to use corticosteroids by mouth for a short period of time. It is important to point out that long-term use of corticosteroids has too many side effects including suppression of the adrenal glands. Given these points, antibiotics such as metronidazole (Flagyl, Metric 21) are useful in improving Crohn’s disease, particularly in the presence of perianal lesions. That is to say, the therapy for each case needs to be tailored according to the physical findings. The physician will customize your treatment accordingly.
Moreover, for more resistant cases the physician might have to resort to immuno-modulating drugs, such as azathioprine (Imuran) or mercaptopurine (brand name: Purinethol) as is described in Ref.12.
Immunosuppressive therapy
The physician can use immunosuppressive therapy with Tacrolimus or cyclosporine. Surprisingly, these drugs are normally used in patients with organ transplants. However, they have been shown to be effective against Crohn’s. For one thing, these are particularly useful in cases where fistulas do not close.
Biologic therapy is the latest, but also most expensive option. Infliximab is an antibody that blocks tumor necrosis factor (TNF), which has been found to be an important cause of Crohn’s. It is administered initially as a series of 3 intravenous injections. For maintenance it has to be given every 8 weeks. This has been shown to induce remission and is also useful in maintaining control of the disease.
Intravenous hyperalimentation
Likewise, for severe cases a period of intravenous hyperalimentation might get the Crohn’s disease more under control and improve the nutritional status. Finally, the surgeon is using surgery only in cases with structural complications; also, where physicians need to reopen blocked passages, close fistulas or take care of abscesses. The surgeon takes care to spare the bowel. If the physician removes too much bowel, this would only worsen the malabsorption syndrome.
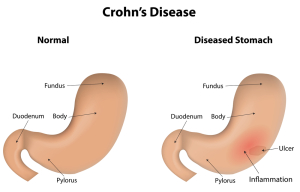
As shown in the image a gastric ulcer can develop as part of Crohn’s disease. This has to be treated with the usual H2-blockers as described under ulcers. In addition, the physician uses the immunomodulatory drugs in the same fashion to keep inflammation from Crohn’s disease under control. The specialist performs a gastroscopy (and possibly an enteroscopy) intermittently for follow-up to ensure that the gastric ulcer is healing and Chrohn’s disease is also under control.
Hormone treatment
Notably, blood tests can determine hormone deficiencies in some patients. When Crohn’s disease develops in women who enter menopause, estrogen and progesterone can be low. For this reason, bio-identical hormone replacement (by way of creams) can improve the inflammatory bowel remarkably. Similarly, low thyroid hormone can also contribute to this illness. In this case replacement with thyroid hormones will lead to further improvement of the bowel condition. Another key point is that in other patients growth hormone can be low. The physician measures it indirectly by its close working partner, somatomedin C. It is important to realize that low-dose growth hormone injections can overcome this deficiency.
Advantage of bioidentical hormone therapy
The advantage of natural hormone therapy is that the body already has the hormone receptors in place, which fit bio-identical hormones. Drugs often have serious side-effects, which limit their application. However, it is wise to use whatever makes the patient better, so this likely would be a combination of several treatment methods.
References
1. M Frevel Aliment Pharmacol Ther 2000 Sep (9): 1151-1157.
2. M Candelli et al. Panminerva Med 2000 Mar 42(1): 55-59.
3. LA Thomas et al. Gastroenterology 2000 Sep 119(3): 806-815.
4. R Tritapepe et al. Panminerva Med 1999 Sep 41(3): 243-246.
5. The Merck Manual, 7th edition, by M. H. Beers et al., Whitehouse Station, N.J., 1999. Chapters 20,23, 26.
6. EJ Simchuk et al. Am J Surg 2000 May 179(5):352-355.
7. G Uomo et al. Ann Ital Chir 2000 Jan/Feb 71(1): 17-21.
8. PG Lankisch et al. Int J Pancreatol 1999 Dec 26(3): 131-136.
9. HB Cook et al. J Gastroenterol Hepatol 2000 Sep 15(9): 1032-1036.
10. W Dickey et al. Am J Gastroenterol 2000 March 95(3): 712-714.
11. M Hummel et al. Diabetologia 2000 Aug 43(8): 1005-1011.
12. DG Bowen et al. Dig Dis Sci 2000 Sep 45(9):1810-1813.
13. The Merck Manual, 7th edition, by M. H. Beers et al., Whitehouse Station, N.J., 1999.Chapter 31, page 311.
14. O Punyabati et al. Indian J Gastroenterol 2000 Jul/Sep 19(3):122-125.
15. S Blomhoff et al. Dig Dis Sci 2000 Jun 45(6): 1160-1165.
16. M Camilleri et al. J Am Geriatr Soc 2000 Sep 48(9):1142-1150.
17. MJ Smith et al. J R Coll Physicians Lond 2000 Sep/Oct 34(5): 448-451.
More references
18. YA Saito et al. Am J Gastroenterol 2000 Oct 95(10): 2816-2824.
19. M Camilleri Am J Med 1999 Nov 107(5A): 27S-32S.
20. CM Prather et al. Gastroenterology 2000 Mar 118(3): 463-468.
21. MJ Farthing : Baillieres Best Pract Res Clin Gastroenterol 1999 Oct 13(3): 461-471.
22. D Heresbach et al. Eur Cytokine Netw 1999 Mar 10(1): 7-15.
23. BE Sands et al. Gastroenterology 1999 Jul 117(1):58-64.
24. B Greenwood-Van Meerveld et al.Lab invest 2000 Aug 80(8):1269-1280.
25. GR Hill et al. Blood 2000 May 1;95(9): 2754-2759.
26. RB Stein et al. Drug Saf 2000 Nov 23(5):429-448.
27. JM Wagner et al. JAMA 1996 Nov 20;276 (19): 1589-1594.
28. James Chin, M.D. Control of Communicable Diseases Manual. 17th ed., American Public Health Association, 2000.
29. The Merck Manual, 7th edition, by M. H. Beers et al., Whitehouse Station, N.J., 1999. Chapter 157, page1181.
30. Textbook of Primary Care Medicine, 3rd ed., Copyright © 2001 Mosby, Inc., pages 976-983: “Chapter 107 – Acute Abdomen and Common Surgical Abdominal Problems”.
31. Marx: Rosen’s Emergency Medicine: Concepts and Clinical Practice, 5th ed., Copyright © 2002 Mosby, Inc. , p. 185:”Abdominal pain”.
32. Feldman: Sleisenger & Fordtran’s Gastrointestinal and Liver Disease, 7th ed., Copyright © 2002 Elsevier, p. 71: “Chapter 4 – Abdominal Pain, Including the Acute Abdomen”.
33. Ferri: Ferri’s Clinical Advisor: Instant Diagnosis and Treatment, 2004 ed., Copyright © 2004 Mosby, Inc.
34. Suzanne Somers: “Breakthrough” Eight Steps to Wellness– Life-altering Secrets from Today’s Cutting-edge Doctors”, Crown Publishers, 2008