A recent pilot clinical trial showed that an ovarian cancer vaccine worked. 25 patients were part of this study to demonstrate whether or not there was toxicity regarding the vaccine. Also, the researchers wanted to know whether the vaccine showed any results.
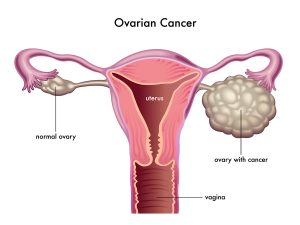
Ovarian cancer diagnosis usually happens only at a later stage of the disease, and at that point it is very difficult to treat. Using combination chemotherapy stage IV ovarian cancer has only a 5-year survival rate of 10%.
The researchers were a team of US and Swiss researchers. They published their results here.
Design of trial
Researchers incubated oxidized whole tumor cell lysate together with the patient’s own dendritic cells from the blood. Dendritic cells are the presenting cells from the immune system. The mix was used as injectable material into lymph nodes of the patients. There the T cells recognized tumor bits and pieces from the dendritic cells as something abnormal. As a result the T cells turn into killer T cells that now attack the remaining ovarian cancer that surgeons had been unable to remove.
Two-year results that showed that the ovarian cancer vaccine worked
78% of those patients who received vaccination in addition to chemotherapy survived at 2 years. Only 44% of those who had received chemotherapy drugs alone, but no vaccine, survived at the 2-year point. There was one patient who had received only the vaccine. She was still in cancer remission 5 years after the completion of the study. All those who had received ovarian cancer vaccine tolerated the injections very well. There were no negative reactions.
Discussion
The objective of this pilot study was to check that it was safe to give an individual ovarian cancer vaccine. Also, the question was whether there would be some tangible results. The study met both of these objectives. The 34% better survival data after 2 years were due to the effect of the ovarian cancer vaccine. Now a much larger study is necessary to check out what therapy is the best, whether it is vaccination alone, vaccination in combinations with chemotherapy or chemotherapy alone. Much larger numbers of patients are necessary to determinate this and perhaps a longer observation period as well. Dr. Lana Kandalaft has already indicated that they will organize a much larger follow-up study, where they hope to receive answers to these questions. It appears that immunotherapy will be at least part of the new treatment modality for ovarian cancer.
Conclusion
A new pilot study has looked into the survival of end-stage ovarian cancer patients. The physicians gave the patients a new individually made ovarian cancer vaccine with or without additional chemotherapy. Their overall survival over 2 years was 34% higher when the cancer vaccine was included. The same research team wants to now do a larger study including more patients and possibly following the patients up after treatment for a longer time. This new cancer vaccine may be a game changer in the treatment of advanced ovarian cancer.