In public language a root canal is the final condition of a severe tooth infection (see below). Medically it is called a pulpitis and this is an inflammation of the dental pulp that develops when tooth decay (caries) is left untreated. It can also follow untreated trauma to a tooth or after extensive restorative work has been done for tooth decay. When a cavity reaches deep into the dentin layer of the tooth or when trauma affects the lymphatic flow or the blood vessels within the root and the pulp of the tooth, pulpitis develops as a reversible condition. When the cavity is repaired by the dentist, the inflammation of the pulp often subsides and the tooth may survive unharmed. If the swelling inside the rigid dentin layer is not subsiding, the circulation through the narrow root canal comes to a stop and the pulp inside the tooth dies off. This is known as irreversible pulpitis and is very susceptible to infection. Dental x-rays help the dentist to assess the extent of the tooth decay and whether or not the alveolar bone has been eroded.
Signs and symptoms
With reversible pulpitis there is hypersensitivity to cold food products or to sweets. When the stimulus is removed by rinsing out the mouth cavity, the pain is gone within 1 to 2 seconds. With irreversible pulpitis the condition is much more difficult to pinpoint as the symptoms are more subtle and confusing. First, there is often a spontaneous onset of pain, but the tooth ache is less well localized. If there is aggravation by cold or hot food, this lingers on for much longer, even when the stimulus is removed. The patient has sometimes difficulties to localize the root canal pain as it is more diffuse in nature and the tooth pain may even switch between the upper and lower teeth, which are either supplied by the maxillary nerve or the mandibular nerve. Interestingly, there is never confusion between right and left. When the nerve is dead, the pain can disappear for a few days, but new pain symptoms arise as complications of super infection set in. As the infection spreads through the apical foramen from inside the tooth to the apex of the tooth, the whole tooth gets lifted from the tooth abscess, which is sensed by the patient as the tooth being “too high” and being painful with every bite. This is an emergency and requires intervention by the dentist. At this late stage the tooth may need to be extracted. If this condition is left untreated this can lead to cellulitis, osteomyelitis, parapharyngeal abscess, mediastinitis, pericarditis and even to a brain abscess or to sepsis.
Treatment
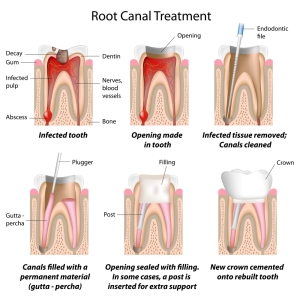
As already discussed, treatment for reversible pulpitis consists of a repair of the cavity and tooth restoration. With irreversible pulpitis root canal treatment (endodontic treatment) is required. This involves the reaming out of the dead pulp including the root canal nerves. Next the root canal is filled with a rubber like substance, called gutta percha, and the tooth is topped with a crown (out of gold or porcelain). When all is done, the patient should no longer have pain and x-rays a few months later would show that all of the radiolucency of the apical bone has normalized.
References:
1. Suzanne Somers: “Breakthrough” Eight Steps to Wellness – Life-altering Secrets from Today’s Cutting-edge Doctors”, Crown Publishers, 2008
2. http://www.webmd.com/oral-health/dental-root-canals
3. http://www.aacd.com/whitening
4. http://www.nhs.uk/conditions/Gum-disease/Pages/Introduction.aspx
5. http://www.aae.org/patients/treatments-and-procedures/root-canals/root-canals.aspx
6. http://en.wikipedia.org/wiki/Dental_trauma
7. http://www.dailymail.co.uk/health/article-25286/The-complete-guide-cosmetic-dentistry.html