Introduction
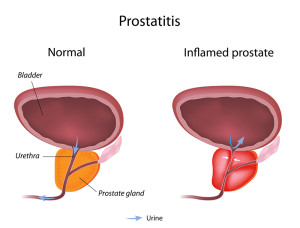
Prostatitis is an inflammation of the tissue of the prostate gland. The prostate gland is situated right underneath the bladder and embraces the upper part of the urethra. Many symptoms can be easily deducted from this knowledge and are somewhat similar to benign prostatic hyperplasia (=BPH). The cause for the inflammation of the prostate (thanks to ccmurology.com for this image) can be bacterial or nonbacterial. It can also be acute or chronic.
Acute prostatitis presents with a high fever and chills, pain in the lower back and in the perineum (the area between the scrotum and the anus).The man also complains about frequent urination with urgency (can’t wait). It often hurts to urinate (called”dysuria”), it might burn and there might be blood in the urine.
If a mild degree of BPH was present before, there may now be a real problem emptying the bladder, occasionally even complete urinary obstruction requiring catheterization. Along with these local symptoms might be some general malaise with joint and muscle aches and pains. The examining physician when doing a gentle rectal exam will find the prostate to be diffusely swollen and tender, warm and occasionally hardened. Often cystitis coexists with the same pathogen and a mid stream urine would then indicate which bacterium is growing. With a very high fever and general malaise, there might be positive blood cultures indicating septicemia.
Chronic prostatitis occurs when the acute prostatitis did not respond to the initial antibiotics. There is a higher chance here that we are now dealing with a nonbacterial prostatitis.
Urologists find this condition frustrating because there is no therapy other than supportive measures to offer, yet the patients have chronic symptoms that mimic those of acute prostatitis. Secretions after a prostate massage, urethral swabs and midstream urine to cover bladder content are all sent for bacterial cultures just to be certain that a chronic bacterial cause was not missed. Ref. 3 shows that Mycoplasma genitalium is one of the pathogens that can cause nongonococcal urethritis and likely is one of the candidates to explain nonbacterial chronic prostatitis as well. Ref. 4 proves that Ureaplasma urealyticum is another cause of chronic prostatitis.
Treatment
Treatment for prostatitis is largely empirical, but based on any positive bacterial cultures as well. For acute prostatitis with septicemia usually intravenous ampicillin and gentamycin are given until the positive cultures come back, at which time the antibiotics are adjusted according to the lab findings.
Antibiotics are continued intravenously for 2 days beyond the point where the patient has no longer a fever. If there is a complete stop of urinary flow, a suprapubic catheter is introduced into the bladder through a small skin and bladder incision. With chronic prostatitis where gram-negative bacteria, chlamydia and enterococci are often found fluoroquinolone, such as ciprofloxacin (brand name: Cipro) or levofloxacin (brand name: Levaquin) or others are given by mouth twice daily for a prolonged period of time (usually 4 to 12 weeks). For chronic nonbacterial prostatitis usually non steroidal anti-inflammatory medications are given for symptomatic relief.
References:
1. DM Thompson: The 46th Annual St. Paul’s Hospital CME Conference for Primary Physicians, Nov. 14-17, 2000, Vancouver/B.C./Canada
2. C Ritenbaugh Curr Oncol Rep 2000 May 2(3): 225-233.
3. PA Totten et al. J Infect Dis 2001 Jan 183(2): 269-276.
4. M Ohkawa et al. Br J Urol 1993 Dec 72(6):918-921.
5. Textbook of Primary Care Medicine, 3rd ed., Copyright © 2001 Mosby, Inc., pages 976-983: “Chapter 107 – Acute Abdomen and Common Surgical Abdominal Problems”.
6. Marx: Rosen’s Emergency Medicine: Concepts and Clinical Practice, 5th ed., Copyright © 2002 Mosby, Inc. , p. 185:”Abdominal pain”.
7. Feldman: Sleisenger & Fordtran’s Gastrointestinal and Liver Disease, 7th ed., Copyright © 2002 Elsevier, p. 71: “Chapter 4 – Abdominal Pain, Including the Acute Abdomen”.
8. Ferri: Ferri’s Clinical Advisor: Instant Diagnosis and Treatment, 2004 ed., Copyright © 2004 Mosby, Inc.