Bladder cancer pathology is important in order for the physician to know what to treat.
Cellular characteristics
The majority of bladder cancer (about 95%) in the U.S. is caused by a histological type called “transitional cell carcinoma”. Another 3% the pathologist calls “squamous cell carcinoma”. The remaining 2% are due to a variety of rare cancers.
Each of these tumors has its own growth characteristics. To complicate matters, there are different grades within one tumor type.
Three grades of bladder cancer
The World Health Organization has defined three grades of bladder cancers: Grade 1 is a cancer with well formed cells that multiply slowly. On the other end of the spectrum is grade 3, which consists of very restless cells that multiply fast and that have a tendency to metastasize earlier. Among the grade 3 category some authorities separate a more benign grade 3a from a much more aggressive grade 3b. The following table shows 2-year survivals of a group of patients from a study where patients with initially local bladder cancers were followed for 2 years. The only difference among the patients was the pathologist’s finding of a different bladder cancer grade.
2-year survivals of bladder cancer due to different grades
Grade 1 : 95 % Grade 2 : 84 %
Grade 3a: 65 % Grade 3b: 17 %
It is clear from this example that cancer researchers must be very cautious when they claim better outcomes with new therapy modalities. They have to ensure that they are comparing groups of patients that have been matched with regard to the cell type, the grade and the stage of the cancer that is being compared. In the past the lack of attention to such details has caused confusion in many instances (Ref.1).
Development of bladder cancer
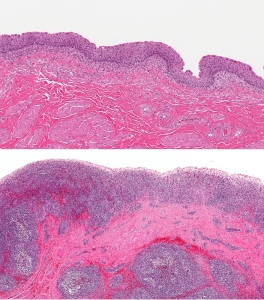
When bladder cancer develops, it does so in a predictable fashion. With the damage of a cancer producing substance (called a “carcinogen”) there is a permanent loss of the most superficial cell layer of the bladder lining.
The body then compensates by increasing the rate of cell division in the deeper layers of the lining and leading to a precancerous condition called “dysplasia”. Severe dysplasia is synonymous with “carcinoma in situ”, a nest of cancer cells in a localized area. Contrary to cancer of the cervix where dysplasia is more localized to one area, with bladder cancer areas of dysplasia develop often simultaneously anywhere in the bladder area and often even anywhere in the urinary tract, from the pelvis of the kidney, the ureter, the bladder and the urethra. This biological fact has practical implications, as the urologist must look at all of the other structures as well during a work-up of bladder cancer in order not to miss an occult second or third lesion! These facts also have implications for bladder cancer recurrences as is illustrated in the following table (Ref.2).
Recurrence rates after excision of superficial bladder cancer
| Margins of tumor specimens found to have… | progression to cancer (%) |
| …normal epithelium | 7 |
| …atypical cells | 36 |
| …carcinoma in situ | 83 |
When a group of patients with carcinoma in situ, proven by biopsy, was followed for 5 years invasive bladder cancer had developed in 39% of patients. The local nest of cancer cells, which is what carcinoma in situ means, does not stay at the surface of the lining of the bladder.
In time it penetrates through the lining into the muscle wall of the bladder and can go all the way through into the surrounding tissues. The cancer cells also have the enzymes to eat their way into lymphatic drainage channels and into blood vessels. This is the beginning of lymph node metastases and distant metastases to other organs leading to end stage cancer.
References
1. Cancer: Principles&Practice of Oncology. 5th edition, volume 1. Edited by Vincent T DeVita, Jr. et al. Lippincott-Raven Publ., Philadelphia,PA, 1997.
2. Cancer: Principles &Practice of Oncology, 4th edition, by V.T. De Vita,Jr.,et al. J.B. LippincottCo.,Philadelphia,1993.Chapter 34, page 1054 (data from text arranged as a table).
3. M Simoneau et al. Oncogene 2000 Dec 19(54): 6317-6323.
4. G Dalbagni , HW Herr Urol Clin North Am 2000 Feb 27(1): 137-146.
5. HW Herr J Clin Oncol 2001 Jan 1;19(1): 89-93.
6. DA Corral, CJ Logothetis World J Urol 1997; 15(2): 139 – 143.
7. PM Dodd et al. J Clin Oncol 1999 Aug;17 (8): 2546- 2552.
8. B. Sears: “The age-free zone”.Regan Books, Harper Collins, 2000.
9. Conn’s Current Therapy 2004, 56th ed., Copyright © 2004 Elsevier
10. Ferri: Ferri’s Clinical Advisor: Instant Diagnosis and Treatment, 2004 ed., Copyright © 2004 Mosby, Inc